Back


Poster Session B - Monday Morning
Category: Esophagus
B0223 - Black Esophagus as Cause of UGIB After a Complicated Urologic Procedure
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Has Audio
- FJ
Fangyuan Jin-Dominguez, MD
Case Western University/UHCMC/Louis Stokes Cleveland VAMC
Cleveland, OH
Presenting Author(s)
Fangyuan Jin-Dominguez, MD1, Umar Hayat, MD2, Emad Mansoor, MD3
1Case Western University/UHCMC/Louis Stokes Cleveland VAMC, Cleveland, OH; 2Case Western University/UHCMC/Louis Stokes VAMC, Cleveland, OH; 3University Hospital Medical Center, Cleveland, OH
Introduction: We report a case of upper endoscopy performed for a patient with coffee-ground emesis after a complicated urologic procedure. It showed diffuse black discoloration in mid-distal esophagus consistent with acute esophageal necrosis (AEN).
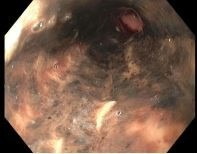
Case Description/Methods: This is a 68-year-old male with diabetes mellitus (DM), chronic kidney disease, hypertension (HTN) and bladder cancer. He was admitted to intensive care after transurethral resection of bladder tumor (TURBT) was complicated by bladder perforation that required open laparotomy and bladder repair. Patient remained intubated for 48 hours. During the postoperative period, he developed ileus with nausea, vomiting and abdominal distention. He subsequently developed coffee-ground emesis and chest pain. He was not on acid suppressing medication. Upper endoscopy was performed to investigate etiology of upper gastrointestinal bleeding (UGIB), which showed diffuse areas of black discoloration in mid-distal esophagus suggestive for esophageal necrosis (Figure 1). Pathology showed tissue necrosis consistent with AEN. Patient was promptly treated with a proton-pump inhibitor and sucralfate. Symptoms rapidly improved without recurrence of bleeding or complication.
Discussion: AEN, also known as “black esophagus” or necrotizing esophagitis, is a rare syndrome characterized by circumferential black mucosa at the distal esophagus and stops at the gastroesophageal junction. The prevalence is about 0.2% and four times more likely in men than women. Risk factors include DM, malignancy, HTN, alcohol abuse and coronary artery disease. The etiology is likely esophageal ischemia from a low-flow state followed by a backflow injury from chemical contents of gastric secretions. Majority of patients present with UGIB, followed by dysphagia and epigastric/chest pain. Symptoms can develop rapidly following an inciting event. With adequate resuscitation and medical therapy (proton pump inhibitors and sucralfate), patients can recover rapidly. Complications may include stricture, perforation, mediastinitis, and death. Prognosis is poor due to underlying critical illness, but mortality specific to AEN is much lower. Endoscopic appearance is suggestive, but biopsy is recommended to establish the diagnosis and exclude other diagnoses (e.g. melanoma and acanthosis nigricans). Repeat endoscopic evaluation is important to assess mucosal healing and determine duration of antacid therapy. Endoscopic balloon dilation may be necessary for stricture from AEN.
Disclosures:
Fangyuan Jin-Dominguez, MD1, Umar Hayat, MD2, Emad Mansoor, MD3. B0223 - Black Esophagus as Cause of UGIB After a Complicated Urologic Procedure, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Case Western University/UHCMC/Louis Stokes Cleveland VAMC, Cleveland, OH; 2Case Western University/UHCMC/Louis Stokes VAMC, Cleveland, OH; 3University Hospital Medical Center, Cleveland, OH
Introduction: We report a case of upper endoscopy performed for a patient with coffee-ground emesis after a complicated urologic procedure. It showed diffuse black discoloration in mid-distal esophagus consistent with acute esophageal necrosis (AEN).
Case Description/Methods: This is a 68-year-old male with diabetes mellitus (DM), chronic kidney disease, hypertension (HTN) and bladder cancer. He was admitted to intensive care after transurethral resection of bladder tumor (TURBT) was complicated by bladder perforation that required open laparotomy and bladder repair. Patient remained intubated for 48 hours. During the postoperative period, he developed ileus with nausea, vomiting and abdominal distention. He subsequently developed coffee-ground emesis and chest pain. He was not on acid suppressing medication. Upper endoscopy was performed to investigate etiology of upper gastrointestinal bleeding (UGIB), which showed diffuse areas of black discoloration in mid-distal esophagus suggestive for esophageal necrosis (Figure 1). Pathology showed tissue necrosis consistent with AEN. Patient was promptly treated with a proton-pump inhibitor and sucralfate. Symptoms rapidly improved without recurrence of bleeding or complication.
Discussion: AEN, also known as “black esophagus” or necrotizing esophagitis, is a rare syndrome characterized by circumferential black mucosa at the distal esophagus and stops at the gastroesophageal junction. The prevalence is about 0.2% and four times more likely in men than women. Risk factors include DM, malignancy, HTN, alcohol abuse and coronary artery disease. The etiology is likely esophageal ischemia from a low-flow state followed by a backflow injury from chemical contents of gastric secretions. Majority of patients present with UGIB, followed by dysphagia and epigastric/chest pain. Symptoms can develop rapidly following an inciting event. With adequate resuscitation and medical therapy (proton pump inhibitors and sucralfate), patients can recover rapidly. Complications may include stricture, perforation, mediastinitis, and death. Prognosis is poor due to underlying critical illness, but mortality specific to AEN is much lower. Endoscopic appearance is suggestive, but biopsy is recommended to establish the diagnosis and exclude other diagnoses (e.g. melanoma and acanthosis nigricans). Repeat endoscopic evaluation is important to assess mucosal healing and determine duration of antacid therapy. Endoscopic balloon dilation may be necessary for stricture from AEN.
Figure: Figure 1: Diffuse circumferential black discoloration in lower esophagus.
Disclosures:
Fangyuan Jin-Dominguez indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Fangyuan Jin-Dominguez, MD1, Umar Hayat, MD2, Emad Mansoor, MD3. B0223 - Black Esophagus as Cause of UGIB After a Complicated Urologic Procedure, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
