Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0267 - The Connections You Don't Want to Make: A Rare Case of Atrio-Esophageal Fistula Formation After Thermal Ablation for Atrial Fibrillation
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- MT
Mahdey Tallat, DO
Staten Island University Hospital
Staten Island, NY
Presenting Author(s)
Mahdey Tallat, DO1, Dhineshreddy Gurala, MD1, Shivantha Amarnath, MD1, Mira Alsheikh, MD1, Aakanksha Sharma, MD2, Youssef Eldouaihy, MD1, Vivek Gumaste, MD1
1Staten Island University Hospital, Staten Island, NY; 2Mount Sinai West, New York, NY
Introduction: Atrio-esophageal fistula (AEF) is a rare yet devastating complication of ablation therapy for atrial fibrillation, with a prevalence of 0.015%-0.04%. Unfortunately, AEF tends to be rapidly fatal without swift recognition and emergent intervention. We present a unique case of AEF in a patient presenting with focal weakness and hemodynamic instability.
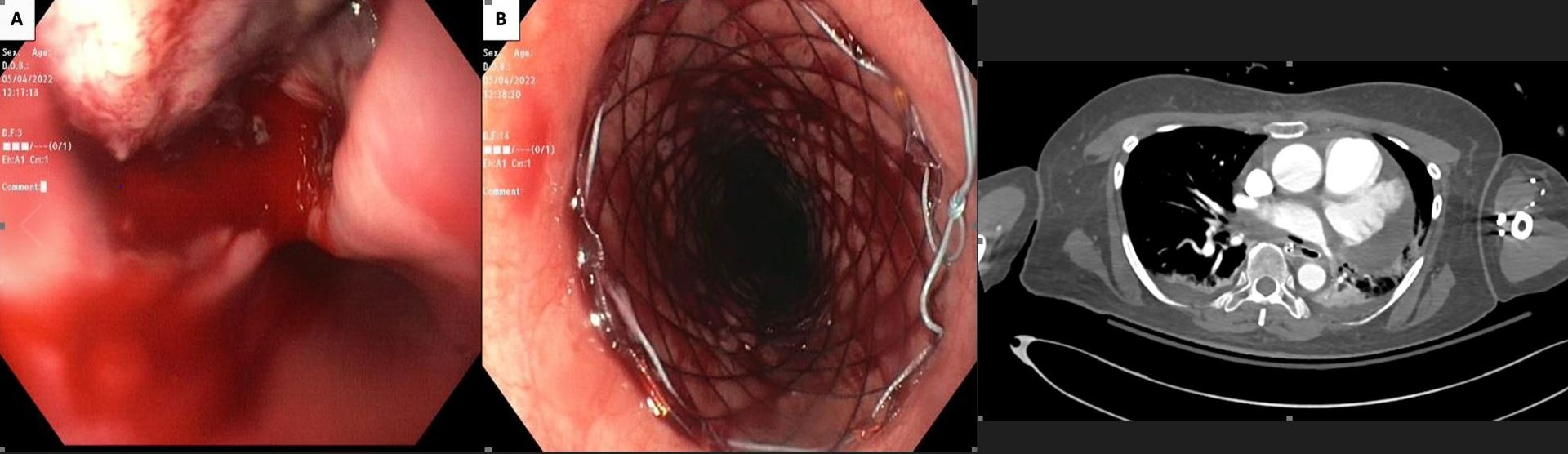
Case Description/Methods: A 65-year-old female with a history of Hypertrophic Cardiomyopathy, Atrial fibrillation on Eliquis who had undergone elective thermal ablation two weeks ago presented to the emergency department with left-sided weakness (NIHSS score of 6). A non-contrast CT head revealed multiple infarcts in the right frontal and cerebellar region. Her hospital course was complicated by recurrent episodes of painless large volume, bright red blood per rectum, fever of 105.7F, and hypotension. A massive transfusion protocol was initiated, and she was intubated for airway protection. An emergent upper endoscopy demonstrated a blood-filled esophagus that was adequately suctioned. A 3cm tear gushing blood in a pulsatile manner was unveiled at the 10 o’clock position, 28cm from the incisors (Image 1). A 20x120mm Through-The-Scope fully covered self-expandable metallic stent was deployed and secured under direct vision with a stent fixation device. After successful hemostasis, she underwent a CT Angiogram of the chest and abdomen, which unveiled air within the left atrium and a defect in the wall suggestive of an AEF (Image 2). Given her rapid deterioration requiring three pressors and persistent bacteremia, she was not a candidate for surgical intervention, and the family opted for palliative extubation and comfort measures.
Discussion: Our case demonstrates the rare yet devastating complication of thermal injury via catheter ablation with the formation of an Atrio-esophageal fistula, which has a mortality rate of up to 80% and usually presents within six weeks of the procedure. Therefore, clinicians should have a high index of suspicion for patients presenting with hematochezia, bacteremia, and neurological symptoms in the setting of ablation therapy. Early recognition and management with antibiotics and surgical repair is the key. In cases where immediate surgery is not feasible, an esophageal stent provides immediate hemostasis.
Disclosures:
Mahdey Tallat, DO1, Dhineshreddy Gurala, MD1, Shivantha Amarnath, MD1, Mira Alsheikh, MD1, Aakanksha Sharma, MD2, Youssef Eldouaihy, MD1, Vivek Gumaste, MD1. C0267 - The Connections You Don't Want to Make: A Rare Case of Atrio-Esophageal Fistula Formation After Thermal Ablation for Atrial Fibrillation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Staten Island University Hospital, Staten Island, NY; 2Mount Sinai West, New York, NY
Introduction: Atrio-esophageal fistula (AEF) is a rare yet devastating complication of ablation therapy for atrial fibrillation, with a prevalence of 0.015%-0.04%. Unfortunately, AEF tends to be rapidly fatal without swift recognition and emergent intervention. We present a unique case of AEF in a patient presenting with focal weakness and hemodynamic instability.
Case Description/Methods: A 65-year-old female with a history of Hypertrophic Cardiomyopathy, Atrial fibrillation on Eliquis who had undergone elective thermal ablation two weeks ago presented to the emergency department with left-sided weakness (NIHSS score of 6). A non-contrast CT head revealed multiple infarcts in the right frontal and cerebellar region. Her hospital course was complicated by recurrent episodes of painless large volume, bright red blood per rectum, fever of 105.7F, and hypotension. A massive transfusion protocol was initiated, and she was intubated for airway protection. An emergent upper endoscopy demonstrated a blood-filled esophagus that was adequately suctioned. A 3cm tear gushing blood in a pulsatile manner was unveiled at the 10 o’clock position, 28cm from the incisors (Image 1). A 20x120mm Through-The-Scope fully covered self-expandable metallic stent was deployed and secured under direct vision with a stent fixation device. After successful hemostasis, she underwent a CT Angiogram of the chest and abdomen, which unveiled air within the left atrium and a defect in the wall suggestive of an AEF (Image 2). Given her rapid deterioration requiring three pressors and persistent bacteremia, she was not a candidate for surgical intervention, and the family opted for palliative extubation and comfort measures.
Discussion: Our case demonstrates the rare yet devastating complication of thermal injury via catheter ablation with the formation of an Atrio-esophageal fistula, which has a mortality rate of up to 80% and usually presents within six weeks of the procedure. Therefore, clinicians should have a high index of suspicion for patients presenting with hematochezia, bacteremia, and neurological symptoms in the setting of ablation therapy. Early recognition and management with antibiotics and surgical repair is the key. In cases where immediate surgery is not feasible, an esophageal stent provides immediate hemostasis.
Figure: Upper endoscopy demonstrating 3cm esophageal tear at the 10 o’clock position in the esophagus, 28 cm from the incisors (Left, A), and status post 20x120mm TTS stent placement covering the tear with successful hemostasis (Center, B). Coronal view of a CT angiogram showing air within the left atrium and a small defect in the esophageal wall suggestive of an atrial-esophageal fistula with esophageal stent placement. Additionally, air seen within the pericardium (Right)
Disclosures:
Mahdey Tallat indicated no relevant financial relationships.
Dhineshreddy Gurala indicated no relevant financial relationships.
Shivantha Amarnath indicated no relevant financial relationships.
Mira Alsheikh indicated no relevant financial relationships.
Aakanksha Sharma indicated no relevant financial relationships.
Youssef Eldouaihy indicated no relevant financial relationships.
Vivek Gumaste indicated no relevant financial relationships.
Mahdey Tallat, DO1, Dhineshreddy Gurala, MD1, Shivantha Amarnath, MD1, Mira Alsheikh, MD1, Aakanksha Sharma, MD2, Youssef Eldouaihy, MD1, Vivek Gumaste, MD1. C0267 - The Connections You Don't Want to Make: A Rare Case of Atrio-Esophageal Fistula Formation After Thermal Ablation for Atrial Fibrillation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
