Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0386 - Switch Biologics or Pursue Surgery? Optimizing Clinical Decision Making in the Treatment of Inflammatory Bowel Diseases
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Preeti Prakash, MD
UCLA
Boston, MA
Presenting Author(s)
Preeti Prakash, MD1, Vivy Cusumano, MD2, Joseph Ebriani, BS3, Jenny Sauk, MD4, Berkeley Limketkai, MD, PhD5
1UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA; 4University of California, Los Angeles, Los Angeles, CA; 5UCLA School of Medicine, Los Angeles, CA
Introduction: Biologics have transformed inflammatory bowel disease (IBD) treatment and decreased the need for surgery. However, many patients fail their first biologic and require alternative agents. With each failure, patients face the decision to switch biologics or pursue surgery. Our aims were to (1) evaluate outcomes of switching biologics or pursuing surgery in patients who fail their first biologic and (2) identify factors that influence these outcomes.
Methods: We performed a chart review of IBD patients who initiated a biologic at a tertiary center between 2015-2021. Demographics, disease characteristics, and treatment course were abstracted. Pathways following biologic initiation included (1) maintenance of first biologic, (2) switch to alternate biologic, or (3) surgery. For those who switched biologics or pursued surgery, an outcome was defined as “positive” (not requiring new biologic) or “negative” (requiring new biologic or surgery) by the last follow-up. Proportion and time-to-event analyses were evaluated. Multivariable Cox regression was used to estimate risk of a “negative” outcome based on demographics, disease duration, location, and behavior.
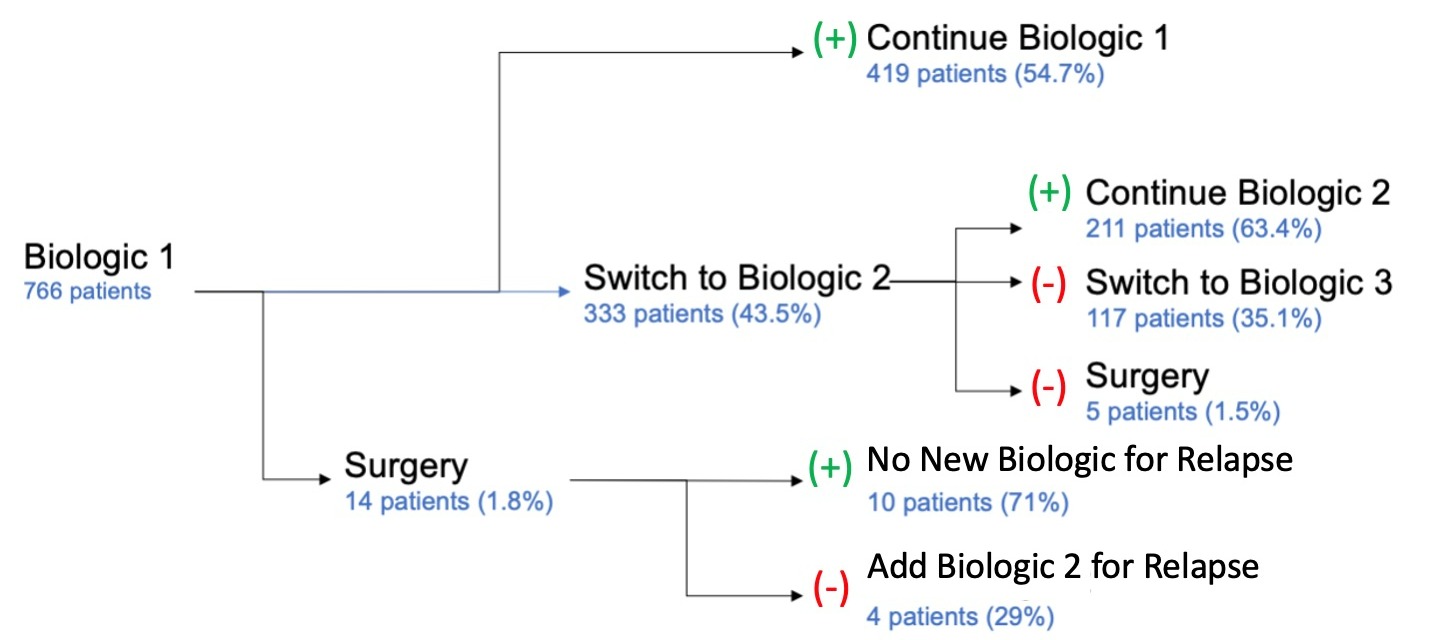
Results: We identified 766 patients who required a biologic with a mean follow-up time of 5.6 years (±4.2). Once initiated on a biologic, the likelihood of continuing the same biologic, switching agents, or requiring surgery were 54.7%, 43.5%, and 1.8%, respectively (Figure). Most patients who switched biologics or underwent surgery after their first biologic ultimately had a “positive” outcome, comparable to the initial biologic (log rank P=0.82). In patients with Crohn’s disease (CD) who switched biologics rather than undergo surgery, stricturing disease (hazard ratio [HR] 3.44, 95% CI 1.56-7.57) and upper gastrointestinal (GI) involvement (HR 9.98, 95% CI 2.35-42.37) correlated with a “negative” outcome. For patients with ulcerative colitis, non-white race (HR 1.34, 95% CI 1.06-1.68) correlated with a “negative” outcome.
Discussion: Half of patients had durable control of disease with their first biologic. For those who failed their first biologic, most switched to a second biologic with a positive outcome, while a minority required surgery. CD stenosis, upper GI involvement, and race were risk factors for treatment failure in patients who switched biologics instead of undergoing surgery. Further investigation is needed to clarify factors that influence medical vs. surgical therapy in patients who fail their first biologic.
Disclosures:
Preeti Prakash, MD1, Vivy Cusumano, MD2, Joseph Ebriani, BS3, Jenny Sauk, MD4, Berkeley Limketkai, MD, PhD5. E0386 - Switch Biologics or Pursue Surgery? Optimizing Clinical Decision Making in the Treatment of Inflammatory Bowel Diseases, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UCLA, Los Angeles, CA; 2University of California Los Angeles, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA; 4University of California, Los Angeles, Los Angeles, CA; 5UCLA School of Medicine, Los Angeles, CA
Introduction: Biologics have transformed inflammatory bowel disease (IBD) treatment and decreased the need for surgery. However, many patients fail their first biologic and require alternative agents. With each failure, patients face the decision to switch biologics or pursue surgery. Our aims were to (1) evaluate outcomes of switching biologics or pursuing surgery in patients who fail their first biologic and (2) identify factors that influence these outcomes.
Methods: We performed a chart review of IBD patients who initiated a biologic at a tertiary center between 2015-2021. Demographics, disease characteristics, and treatment course were abstracted. Pathways following biologic initiation included (1) maintenance of first biologic, (2) switch to alternate biologic, or (3) surgery. For those who switched biologics or pursued surgery, an outcome was defined as “positive” (not requiring new biologic) or “negative” (requiring new biologic or surgery) by the last follow-up. Proportion and time-to-event analyses were evaluated. Multivariable Cox regression was used to estimate risk of a “negative” outcome based on demographics, disease duration, location, and behavior.
Results: We identified 766 patients who required a biologic with a mean follow-up time of 5.6 years (±4.2). Once initiated on a biologic, the likelihood of continuing the same biologic, switching agents, or requiring surgery were 54.7%, 43.5%, and 1.8%, respectively (Figure). Most patients who switched biologics or underwent surgery after their first biologic ultimately had a “positive” outcome, comparable to the initial biologic (log rank P=0.82). In patients with Crohn’s disease (CD) who switched biologics rather than undergo surgery, stricturing disease (hazard ratio [HR] 3.44, 95% CI 1.56-7.57) and upper gastrointestinal (GI) involvement (HR 9.98, 95% CI 2.35-42.37) correlated with a “negative” outcome. For patients with ulcerative colitis, non-white race (HR 1.34, 95% CI 1.06-1.68) correlated with a “negative” outcome.
Discussion: Half of patients had durable control of disease with their first biologic. For those who failed their first biologic, most switched to a second biologic with a positive outcome, while a minority required surgery. CD stenosis, upper GI involvement, and race were risk factors for treatment failure in patients who switched biologics instead of undergoing surgery. Further investigation is needed to clarify factors that influence medical vs. surgical therapy in patients who fail their first biologic.
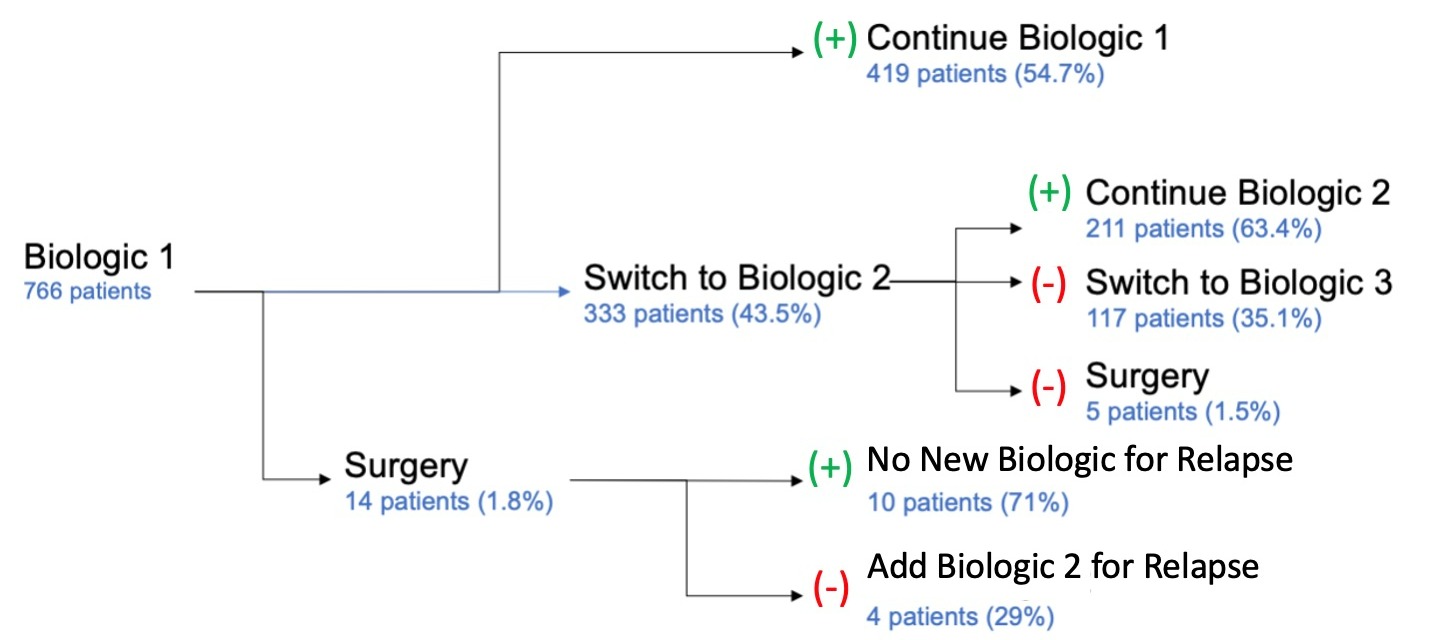
Figure: Figure. Flow chart outlining the course of treatment for patients with IBD who required initiation of a biologic agent
Disclosures:
Preeti Prakash indicated no relevant financial relationships.
Vivy Cusumano indicated no relevant financial relationships.
Joseph Ebriani indicated no relevant financial relationships.
Jenny Sauk: Abbvie – Speakers Bureau. CorEvitas – Consultant. Prometheus – Advisory Committee/Board Member.
Berkeley Limketkai: Azora Therapeutics – Stock-privately held company.
Preeti Prakash, MD1, Vivy Cusumano, MD2, Joseph Ebriani, BS3, Jenny Sauk, MD4, Berkeley Limketkai, MD, PhD5. E0386 - Switch Biologics or Pursue Surgery? Optimizing Clinical Decision Making in the Treatment of Inflammatory Bowel Diseases, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
