Back

Poster Session B - Monday Morning
Category: Stomach
B0708 - Gastric Outlet Obstruction Due to a Large Paraesophageal Hernia: An Uncommon Etiology with Fatal Consequences
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Herman Suga, DO
Jefferson Health New Jersey
Turnersville, NJ
Presenting Author(s)
Herman Suga, DO1, Neethi Dasu, DO2, David J. Truscello, DO1, Kirti Dasu, BA3, Drew Chiesa, DO1, Richard Walters, DO1
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health New Jersey, Voorhees, NJ; 3Drexel Graduate School of Biomedical Sciences and Professional Studies, Philadelphia, PA
Introduction: Paraesophageal hernias are known to be relatively benign and asymptomatic and account for 5% of all hiatal hernias. Patients often present with vague abdominal symptoms such as GERD, nausea, vomiting, postprandial pain, dysphagia and in severe cases hematemesis. Complications with paraesophageal hernias include gastric mucosal necrosis, perforations, strangulation, erosive ulcers and gastric volvulus. We present a case of an 84 year old female with a large paraesophageal hernia causing gastric outlet obstruction ultimately requiring surgery.
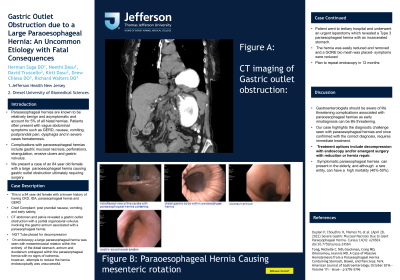
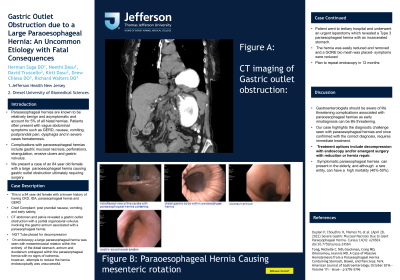
Case Description/Methods: This is a 84 year old female with a known history of having CKD, IDA, paraesophageal hernia and GERD who presented to the hospital for evaluation of post prandial nausea, vomiting, and early satiety, which has been ongoing for a week. She denied having hematemesis or weight loss. On a physical exam, her abdomen was distended but with no tenderness or guarding. CT abdomen and pelvis revealed a gastric outlet obstruction with a partial organoaxial volvulus involving the gastric antrum associated with a paraesophageal hernia. A nasogastric tube was placed for decompression and the patient was taken to endoscopy the following day. On endoscopy a large paraesophageal hernia was seen with mesenteroaxial rotation within the entirety of the distal stomach, antrum and duodenum entrapped within the paraesophageal hernia with no signs of ischemia, however, attempts to reduce the hernia endoscopically was unsuccessful. The patient was transferred to a tertiary hospital and underwent an urgent laparotomy which revealed a Type 3 paraesophageal hernia with an incarcerated stomach. The hernia was easily reduced and removed and a GORE bio mesh was placed. Her symptoms improved greatly post-operatively with a plan to have a repeat endoscopy in 12 months.
Discussion: Gastroenterologists should be aware of life threatening complications associated with paraesophageal hernias as early misdiagnosis can be life threatening. Our case highlights the diagnostic challenge seen with paraesophageal hernias and once confirmed with the correct diagnosis, requires immediate treatment. Treatment options include decompression with endoscopy and/or emergent surgery with reduction or hernia repair. Symptomatic paraesophageal hernias can present in the elderly, and although a rare entity, can have a high mortality (40%-50%).

Disclosures:
Herman Suga, DO1, Neethi Dasu, DO2, David J. Truscello, DO1, Kirti Dasu, BA3, Drew Chiesa, DO1, Richard Walters, DO1. B0708 - Gastric Outlet Obstruction Due to a Large Paraesophageal Hernia: An Uncommon Etiology with Fatal Consequences, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health New Jersey, Voorhees, NJ; 3Drexel Graduate School of Biomedical Sciences and Professional Studies, Philadelphia, PA
Introduction: Paraesophageal hernias are known to be relatively benign and asymptomatic and account for 5% of all hiatal hernias. Patients often present with vague abdominal symptoms such as GERD, nausea, vomiting, postprandial pain, dysphagia and in severe cases hematemesis. Complications with paraesophageal hernias include gastric mucosal necrosis, perforations, strangulation, erosive ulcers and gastric volvulus. We present a case of an 84 year old female with a large paraesophageal hernia causing gastric outlet obstruction ultimately requiring surgery.
Case Description/Methods: This is a 84 year old female with a known history of having CKD, IDA, paraesophageal hernia and GERD who presented to the hospital for evaluation of post prandial nausea, vomiting, and early satiety, which has been ongoing for a week. She denied having hematemesis or weight loss. On a physical exam, her abdomen was distended but with no tenderness or guarding. CT abdomen and pelvis revealed a gastric outlet obstruction with a partial organoaxial volvulus involving the gastric antrum associated with a paraesophageal hernia. A nasogastric tube was placed for decompression and the patient was taken to endoscopy the following day. On endoscopy a large paraesophageal hernia was seen with mesenteroaxial rotation within the entirety of the distal stomach, antrum and duodenum entrapped within the paraesophageal hernia with no signs of ischemia, however, attempts to reduce the hernia endoscopically was unsuccessful. The patient was transferred to a tertiary hospital and underwent an urgent laparotomy which revealed a Type 3 paraesophageal hernia with an incarcerated stomach. The hernia was easily reduced and removed and a GORE bio mesh was placed. Her symptoms improved greatly post-operatively with a plan to have a repeat endoscopy in 12 months.
Discussion: Gastroenterologists should be aware of life threatening complications associated with paraesophageal hernias as early misdiagnosis can be life threatening. Our case highlights the diagnostic challenge seen with paraesophageal hernias and once confirmed with the correct diagnosis, requires immediate treatment. Treatment options include decompression with endoscopy and/or emergent surgery with reduction or hernia repair. Symptomatic paraesophageal hernias can present in the elderly, and although a rare entity, can have a high mortality (40%-50%).

Figure: Endoscopy and CT images of paraesophageal hernia causing gastric outlet obstruction
Disclosures:
Herman Suga indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
David Truscello indicated no relevant financial relationships.
Kirti Dasu indicated no relevant financial relationships.
Drew Chiesa indicated no relevant financial relationships.
Richard Walters indicated no relevant financial relationships.
Herman Suga, DO1, Neethi Dasu, DO2, David J. Truscello, DO1, Kirti Dasu, BA3, Drew Chiesa, DO1, Richard Walters, DO1. B0708 - Gastric Outlet Obstruction Due to a Large Paraesophageal Hernia: An Uncommon Etiology with Fatal Consequences, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
