Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0392 - Importance of Bifidobacteria in Crohn’s Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sabine Hazan, MD
ProgenaBiome, LLC
VENTURA, CA
Presenting Author(s)
Sabine Hazan, MD1, Sonya Dave, PhD2, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG3
1ProgenaBiome, LLC, Ventura, CA; 2North End Advisory, Smyrna, GA; 3Centre for Digestive Diseases, Five Dock, New South Wales, Australia
Introduction: Crohn’s disease is an inflammatory bowel disease thought to be multifactorial in etiology from microbiome disruption to infectious process to genetics. The prevalence of Crohn’s is around 180/100,000 in 2016 and healthcare burden in the billions of dollars.
Studies by Bozkurt et al. showed that intracolonic administration of certain bifidobacteria species resolved inflammatory bowel disease symptoms and improved mucosal healing. Studies by Paramsothy, Borody and colleagues on fecal transplant showed improved outcomes in ulcerative colitis compared to placebo. In view of these potential breakthrough therapies, we sought to investigate the relative abundance of genus bifidobacterium in patients virgin to treatment compared to patients in treatment compared to healthy controls.
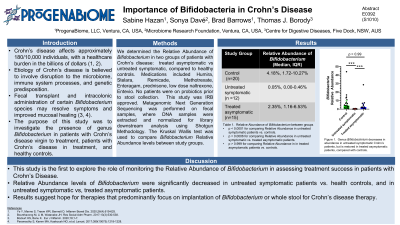
Methods: We determined Relative Abundance of bifidobacteria in two groups of Crohn’s patients: treated asymptomatic vs untreated symptomatic, compared to healthy controls. Medications included Humira, Stelara, Remicade, Methotrexate, Enteragam, prednisone, low dose naltrexone, Entevio). No patients in all three groups were on probiotics prior to stool collection. Metagenomic Next Generation Sequencing was performed on fecal samples, where DNA samples were extracted and normalized for library downstream analysis using Shotgun Methodology. The Kruskal-Wallis test was used for comparison.
This study was IRB approved.
Results: Relative Abundance of Bifidobacterium levels significantly decreased in untreated symptomatic Crohn’s patients vs. control ( p< 0.0001) and in untreated symptomatic vs. treated asymptomatic ( p = 0.0006). No significant difference was observed between medicated asymptomatic vs. healthy control (p > 0.999). Median, interquartile range and sample size of groups were: control (4.18%, 1.72-10.27%, n =20), untreated (0.05%, 0.00-0.46%, n=12) and treated (2.35%, 1.16-6.53%, n=15). These results were highly significant despite small sample sizes.
Discussion: This is the first study to explore the role of monitoring the relative abundance of bifidobacteria in assessing treatment success in Crohn’s patients. Although a small study, it does show hope for therapies that predominantly focus on implantation of the species of Bifidobacteria or whole stool as part of Crohn’s therapy.

Disclosures:
Sabine Hazan, MD1, Sonya Dave, PhD2, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG3. E0392 - Importance of Bifidobacteria in Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1ProgenaBiome, LLC, Ventura, CA; 2North End Advisory, Smyrna, GA; 3Centre for Digestive Diseases, Five Dock, New South Wales, Australia
Introduction: Crohn’s disease is an inflammatory bowel disease thought to be multifactorial in etiology from microbiome disruption to infectious process to genetics. The prevalence of Crohn’s is around 180/100,000 in 2016 and healthcare burden in the billions of dollars.
Studies by Bozkurt et al. showed that intracolonic administration of certain bifidobacteria species resolved inflammatory bowel disease symptoms and improved mucosal healing. Studies by Paramsothy, Borody and colleagues on fecal transplant showed improved outcomes in ulcerative colitis compared to placebo. In view of these potential breakthrough therapies, we sought to investigate the relative abundance of genus bifidobacterium in patients virgin to treatment compared to patients in treatment compared to healthy controls.
Methods: We determined Relative Abundance of bifidobacteria in two groups of Crohn’s patients: treated asymptomatic vs untreated symptomatic, compared to healthy controls. Medications included Humira, Stelara, Remicade, Methotrexate, Enteragam, prednisone, low dose naltrexone, Entevio). No patients in all three groups were on probiotics prior to stool collection. Metagenomic Next Generation Sequencing was performed on fecal samples, where DNA samples were extracted and normalized for library downstream analysis using Shotgun Methodology. The Kruskal-Wallis test was used for comparison.
This study was IRB approved.
Results: Relative Abundance of Bifidobacterium levels significantly decreased in untreated symptomatic Crohn’s patients vs. control ( p< 0.0001) and in untreated symptomatic vs. treated asymptomatic ( p = 0.0006). No significant difference was observed between medicated asymptomatic vs. healthy control (p > 0.999). Median, interquartile range and sample size of groups were: control (4.18%, 1.72-10.27%, n =20), untreated (0.05%, 0.00-0.46%, n=12) and treated (2.35%, 1.16-6.53%, n=15). These results were highly significant despite small sample sizes.
Discussion: This is the first study to explore the role of monitoring the relative abundance of bifidobacteria in assessing treatment success in Crohn’s patients. Although a small study, it does show hope for therapies that predominantly focus on implantation of the species of Bifidobacteria or whole stool as part of Crohn’s therapy.

Figure: Figure 1: Genus Bifidobacteria decreases in abundance in untreated symptomatic Crohn’s patients, but is restored in treated asymptomatic patients, compared with controls.
Disclosures:
Sabine Hazan indicated no relevant financial relationships.
Sonya Dave: McKesson Specialty Health / Ontada – Employee.
Brad Barrows indicated no relevant financial relationships.
Thomas Borody: Axent medical Pty. Ltd – Advisory Committee/Board Member. Centre for Digestive Diseases – Advisory Committee/Board Member, Consultant, Employee, Grant/Research Support, Intellectual Property/Patents, Ownership interest, Owner/Ownership Interest, Stock-privately held company. Finch Therapeutics – Advisory Committee/Board Member, Intellectual Property/Patents, Stock-publicly held company(excluding mutual/index funds). Topelia Therapeutics – Advisor or Review Panel Member, Intellectual Property/Patents.
Sabine Hazan, MD1, Sonya Dave, PhD2, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG3. E0392 - Importance of Bifidobacteria in Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
