Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0393 - Risk of Avoidant/Restrictive Food Intake Disorder Prevalence Among Underrepresented Minority Patients With Inflammatory Bowel Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Konstantinos C. Hantzidiamantis, MD
Boston University Medical Center
Boston, MA
Presenting Author(s)
Award: Presidential Poster Award
Konstantinos Hantzidiamantis, MD1, Shreya Vinjamuri, BA1, Soobin Song, BSc1, Deniz Gaberz-Mah, BSc1, Antonio Lozano, BSc1, Monia Werlang, MD2, Francis A. Farraye, MD, MSc2, Sharmeel K. Wasan, MD3
1Boston University Medical Center, Boston, MA; 2Mayo Clinic, Jacksonville, FL; 3Boston Medical Center, Boston, MA
Introduction: In avoidant/restrictive food intake disorder (ARFID), a newer diagnosis included in the DSM-5, food intake is restricted or avoided based on a disinterest in food, characteristics, or negative experiences associated with food. Recent studies have shown a significantly higher rate of ARFID in patients with inflammatory bowel disease (IBD)1 though these studies have lacked racial and ethnic diversity. Our study aimed to determine if Under Represented Minority (URM) patients with IBD have differing risk for ARFID compared with Caucasian patients.
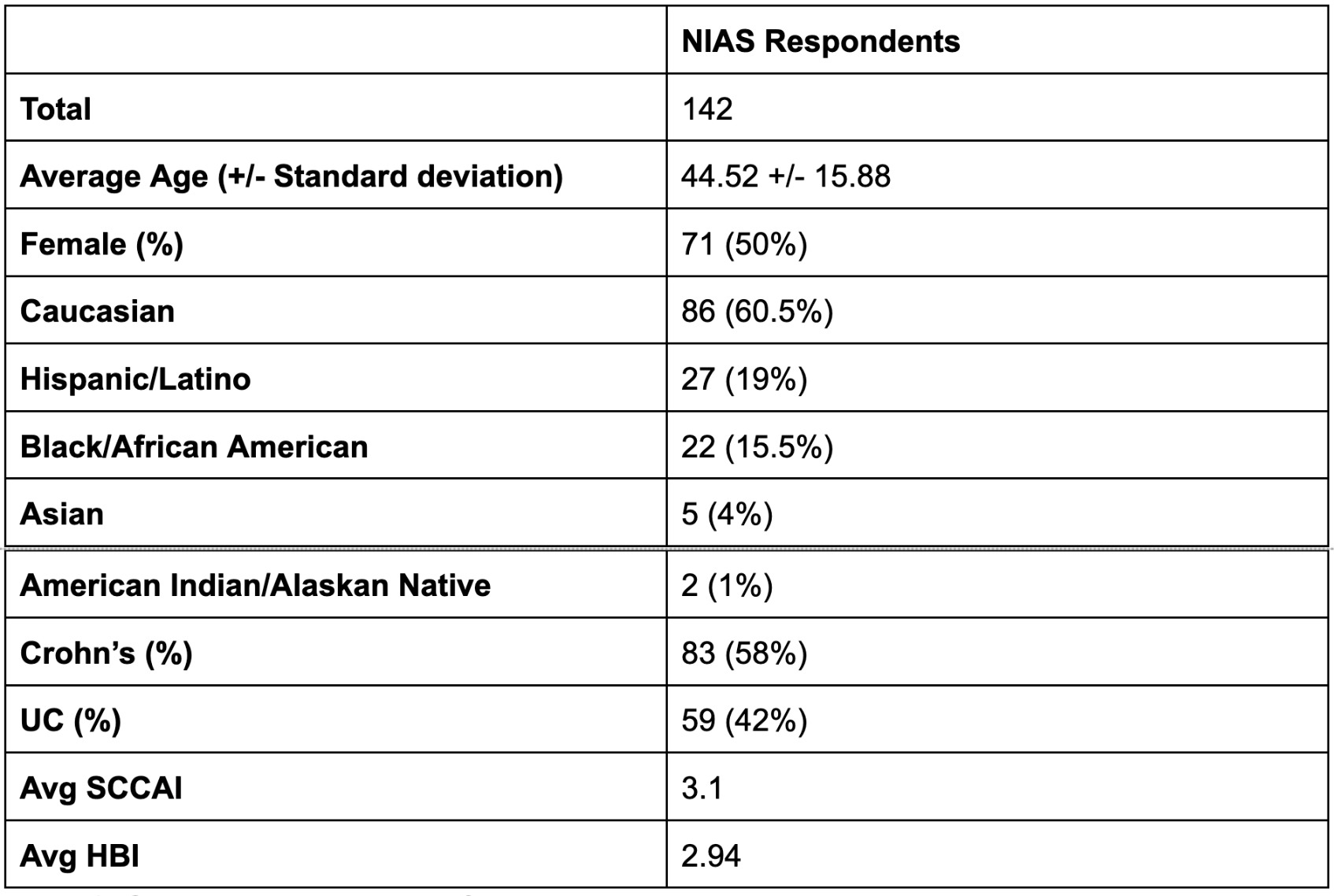
Methods: In this single center, cross sectional study performed at the Clinic for Digestive Diseases at Boston Medical Center, adult patients who carried either a diagnosis of Crohn's disease (CD) or ulcerative colitis (UC) were consented to participate during their office visits. They were administered a Nine Item ARFID Screen (NIAS) and either the Simple Clinical Colitis Index (SCCAI) for UC or the Harvey-Bradshaw Index (HBI) for CD. A score equal to or higher than 24 on the NIAS was considered positive screening for risk of ARFID.2
Results: 11/59 (18.6%) UC patients screened positive for risk of ARFID, while 17/83 (20%) CD patients screened positive. CD patients with a positive risk for ARFID had an average HBI score of 5.4 vs CD patients with low risk for ARFID (average HBI score of 2.3 (p=0.0067)). NIAS + UC patients had an average SCCAI score of 4.4 vs NIAS – UC patients (average SCCAI score of 2.9 (p=0.04)).
URMs had a slightly higher risk for ARFID vs. Caucasians (11/49 (22%) vs 17/86 (19%)). When comparing average NIAS scores among the two populations, Black and Hispanic patients had an average score of 17.04 while Caucasian patients had an average score of 14.05 (p=0.082).
Discussion: Prior studies have noted higher rates of ARFID among Caucasian patients with IBD.1 This study demonstrates that both Caucasian and URM patients with IBD have higher risk for ARFID compared to the general population. Patients with more active CD also had higher NIAS scores. There was a trend toward higher average NIAS scores in URM patients compared to Caucasian patients. Further studies to identify reasons for this trend, such as possible cultural differences in diet addressed during office visits, should be explored.
References
1.) Yelencich et al., Clinical Gastroenterology and Hepatology. 2021, 20(6), 1282-1289
2.) Zickgraf H.F. Ellis J.M. Appetite. 2018, 123, 32-42
Disclosures:
Konstantinos Hantzidiamantis, MD1, Shreya Vinjamuri, BA1, Soobin Song, BSc1, Deniz Gaberz-Mah, BSc1, Antonio Lozano, BSc1, Monia Werlang, MD2, Francis A. Farraye, MD, MSc2, Sharmeel K. Wasan, MD3. E0393 - Risk of Avoidant/Restrictive Food Intake Disorder Prevalence Among Underrepresented Minority Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Konstantinos Hantzidiamantis, MD1, Shreya Vinjamuri, BA1, Soobin Song, BSc1, Deniz Gaberz-Mah, BSc1, Antonio Lozano, BSc1, Monia Werlang, MD2, Francis A. Farraye, MD, MSc2, Sharmeel K. Wasan, MD3
1Boston University Medical Center, Boston, MA; 2Mayo Clinic, Jacksonville, FL; 3Boston Medical Center, Boston, MA
Introduction: In avoidant/restrictive food intake disorder (ARFID), a newer diagnosis included in the DSM-5, food intake is restricted or avoided based on a disinterest in food, characteristics, or negative experiences associated with food. Recent studies have shown a significantly higher rate of ARFID in patients with inflammatory bowel disease (IBD)1 though these studies have lacked racial and ethnic diversity. Our study aimed to determine if Under Represented Minority (URM) patients with IBD have differing risk for ARFID compared with Caucasian patients.
Methods: In this single center, cross sectional study performed at the Clinic for Digestive Diseases at Boston Medical Center, adult patients who carried either a diagnosis of Crohn's disease (CD) or ulcerative colitis (UC) were consented to participate during their office visits. They were administered a Nine Item ARFID Screen (NIAS) and either the Simple Clinical Colitis Index (SCCAI) for UC or the Harvey-Bradshaw Index (HBI) for CD. A score equal to or higher than 24 on the NIAS was considered positive screening for risk of ARFID.2
Results: 11/59 (18.6%) UC patients screened positive for risk of ARFID, while 17/83 (20%) CD patients screened positive. CD patients with a positive risk for ARFID had an average HBI score of 5.4 vs CD patients with low risk for ARFID (average HBI score of 2.3 (p=0.0067)). NIAS + UC patients had an average SCCAI score of 4.4 vs NIAS – UC patients (average SCCAI score of 2.9 (p=0.04)).
URMs had a slightly higher risk for ARFID vs. Caucasians (11/49 (22%) vs 17/86 (19%)). When comparing average NIAS scores among the two populations, Black and Hispanic patients had an average score of 17.04 while Caucasian patients had an average score of 14.05 (p=0.082).
Discussion: Prior studies have noted higher rates of ARFID among Caucasian patients with IBD.1 This study demonstrates that both Caucasian and URM patients with IBD have higher risk for ARFID compared to the general population. Patients with more active CD also had higher NIAS scores. There was a trend toward higher average NIAS scores in URM patients compared to Caucasian patients. Further studies to identify reasons for this trend, such as possible cultural differences in diet addressed during office visits, should be explored.
References
1.) Yelencich et al., Clinical Gastroenterology and Hepatology. 2021, 20(6), 1282-1289
2.) Zickgraf H.F. Ellis J.M. Appetite. 2018, 123, 32-42
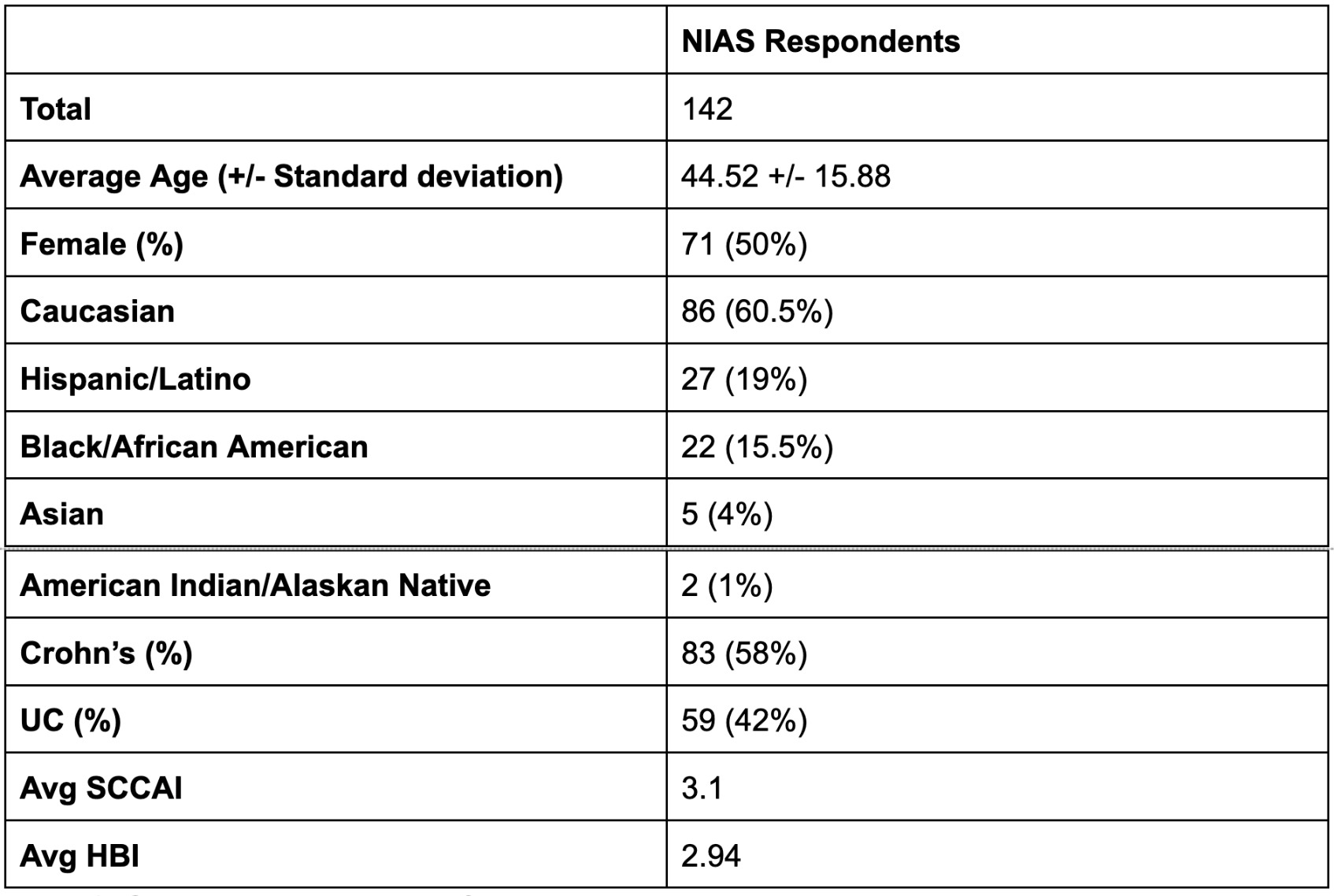
Figure: Table 1: General Demographic Information
Disclosures:
Konstantinos Hantzidiamantis indicated no relevant financial relationships.
Shreya Vinjamuri indicated no relevant financial relationships.
Soobin Song indicated no relevant financial relationships.
Deniz Gaberz-Mah indicated no relevant financial relationships.
Antonio Lozano indicated no relevant financial relationships.
Monia Werlang indicated no relevant financial relationships.
Francis Farraye: Adiso Therapeutics – DSMB. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. GSK – Advisory Committee/Board Member. IBD Educational Group – Advisory Committee/Board Member. Innovation Pharmaceuticals – Stock Options. Iterative Scopes – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Theravance – DSMB.
Sharmeel Wasan: Pfizer – Grant/Research Support.
Konstantinos Hantzidiamantis, MD1, Shreya Vinjamuri, BA1, Soobin Song, BSc1, Deniz Gaberz-Mah, BSc1, Antonio Lozano, BSc1, Monia Werlang, MD2, Francis A. Farraye, MD, MSc2, Sharmeel K. Wasan, MD3. E0393 - Risk of Avoidant/Restrictive Food Intake Disorder Prevalence Among Underrepresented Minority Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


