Back

Poster Session A - Sunday Afternoon
Category: Colon
A0138 - Glucagon-Like Peptide-1 Receptor Agonist-Associated Colonic Ischemia: A Case Report
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Thomas A. Wichelmann, DO
Advocate Lutheran General Hospital
Park Ridge, IL
Presenting Author(s)
Thomas A. Wichelmann, DO1, David H. Kruchko, DO1, Dean Silas, MD2
1Advocate Lutheran General Hospital, Park Ridge, IL; 2Advocate Lutheran General Hospital, Niles, IL
Introduction: Colonic ischemia is a well-recognized disease process with both modifiable and non-modifiable risk factors. While most cases are mild and self-limited, some patients experience significant distress requiring hospitalization, surgery, and rarely death. Recognizing and preventing modifiable risk factors is paramount.
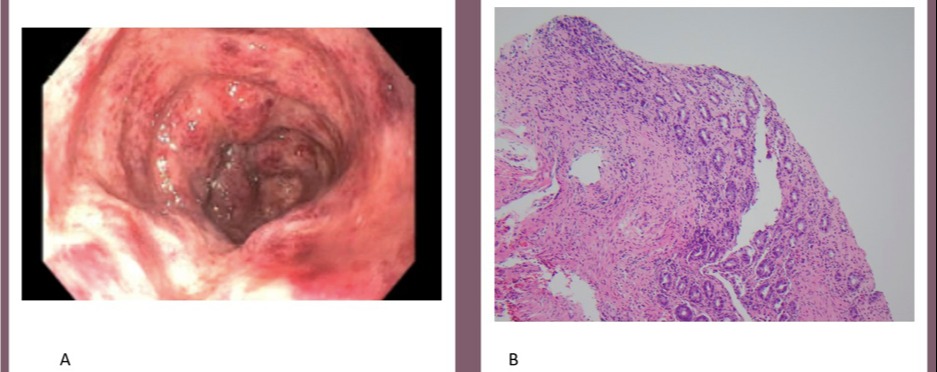
Case Description/Methods: A healthy 56-year-old female presented to the emergency department with 10 days of worsening bright red blood per rectum, tenesmus, and intermittent upper abdominal pain. She denied any other symptoms or recent travel. Two months prior she was started on weekly 0.25 mg subcutaneous semaglutide injections for weight loss. She described decreased thirst and appetite since starting the medication. Her last colonoscopy was 2 years prior and unremarkable. Presenting vital signs were stable with no documented hypotension. BMI was 27 kg/m². Physical exam was unremarkable. Patient's blood work was unrevealing, including normal lactic acid. CT abdomen pelvis with IV contrast showed isolated acute sigmoid colitis and mesenteric duplex was negative for ischemia. MRI was performed of the abdomen due to concern for portal vein clot on CT scan which confirmed portal vein thrombus. Hematology was consulted, the patient was started on full dose anticoagulation, and coagulopathy workup was unrevealing suggesting the clot was a manifestation of colonic ischemia. Infectious stool studies were negative. Flexible sigmoidoscopy revealed severe localized inflammation in the mid sigmoid colon (Image 1A). Biopsies demonstrated colonic mucosa with focal lamina propria fibrosis, hemorrhage, and reactive regenerative changes, suggestive of ischemic colitis (Image 1B). The patient improved with intravenous fluids and antibiotics to prevent bacterial translocation. She was discharged home on day three with the recommendation for indefinite semaglutide discontinuation.
Discussion: There are no known reports of high-dose GLP-1 receptor agonists (GLP-1-RAs) leading to colonic ischemia when taken for weight loss. Multiple potential mechanisms exist including periods of hypotension due to decreased food and water intake. Further, delayed gastric emptying is a known feature of GLP-1-RAs and can be a manifestation of decreased gastric vascular supply. Interestingly, experimental intestinal ischemia demonstrated rapidly increased GLP-1 levels suggesting a possible correlation. Further investigation into the safety of high dose GLP-1 RAs for weight loss is recommended.
Disclosures:
Thomas A. Wichelmann, DO1, David H. Kruchko, DO1, Dean Silas, MD2. A0138 - Glucagon-Like Peptide-1 Receptor Agonist-Associated Colonic Ischemia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Advocate Lutheran General Hospital, Park Ridge, IL; 2Advocate Lutheran General Hospital, Niles, IL
Introduction: Colonic ischemia is a well-recognized disease process with both modifiable and non-modifiable risk factors. While most cases are mild and self-limited, some patients experience significant distress requiring hospitalization, surgery, and rarely death. Recognizing and preventing modifiable risk factors is paramount.
Case Description/Methods: A healthy 56-year-old female presented to the emergency department with 10 days of worsening bright red blood per rectum, tenesmus, and intermittent upper abdominal pain. She denied any other symptoms or recent travel. Two months prior she was started on weekly 0.25 mg subcutaneous semaglutide injections for weight loss. She described decreased thirst and appetite since starting the medication. Her last colonoscopy was 2 years prior and unremarkable. Presenting vital signs were stable with no documented hypotension. BMI was 27 kg/m². Physical exam was unremarkable. Patient's blood work was unrevealing, including normal lactic acid. CT abdomen pelvis with IV contrast showed isolated acute sigmoid colitis and mesenteric duplex was negative for ischemia. MRI was performed of the abdomen due to concern for portal vein clot on CT scan which confirmed portal vein thrombus. Hematology was consulted, the patient was started on full dose anticoagulation, and coagulopathy workup was unrevealing suggesting the clot was a manifestation of colonic ischemia. Infectious stool studies were negative. Flexible sigmoidoscopy revealed severe localized inflammation in the mid sigmoid colon (Image 1A). Biopsies demonstrated colonic mucosa with focal lamina propria fibrosis, hemorrhage, and reactive regenerative changes, suggestive of ischemic colitis (Image 1B). The patient improved with intravenous fluids and antibiotics to prevent bacterial translocation. She was discharged home on day three with the recommendation for indefinite semaglutide discontinuation.
Discussion: There are no known reports of high-dose GLP-1 receptor agonists (GLP-1-RAs) leading to colonic ischemia when taken for weight loss. Multiple potential mechanisms exist including periods of hypotension due to decreased food and water intake. Further, delayed gastric emptying is a known feature of GLP-1-RAs and can be a manifestation of decreased gastric vascular supply. Interestingly, experimental intestinal ischemia demonstrated rapidly increased GLP-1 levels suggesting a possible correlation. Further investigation into the safety of high dose GLP-1 RAs for weight loss is recommended.
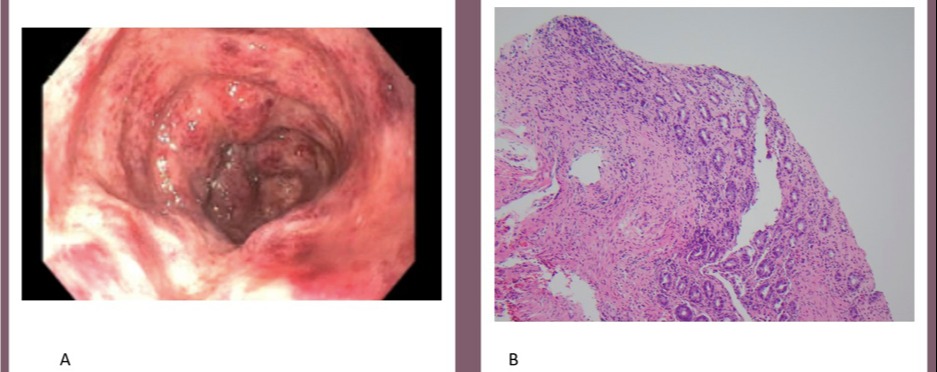
Figure: Image 1, A & B. A: Flexible sigmoidoscopy showing severe inflammation isolated to the sigmoid colon with loss of vascularity, friability, edema, erythema, and mucous. B: Pathology findings demonstrating focal lamina propria fibrosis, hemorrhage and reactive regenerative changes, suggestive of colonic ischemia.
Disclosures:
Thomas Wichelmann indicated no relevant financial relationships.
David Kruchko indicated no relevant financial relationships.
Dean Silas indicated no relevant financial relationships.
Thomas A. Wichelmann, DO1, David H. Kruchko, DO1, Dean Silas, MD2. A0138 - Glucagon-Like Peptide-1 Receptor Agonist-Associated Colonic Ischemia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

