Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0330 - Brunner’s Gland Hyperplastic Polyp Resulting in Gastrointestinal Bleeding: A Zebra Does Not Change Its Stripes!
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- HS
Hassan M. Shaheen, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Hassan M. Shaheen, MD, Ashraf Almomani, MD, Prabhat Kumar, MD, Antoine Boustany, MD, MPH, Eduard Krishtopaytis, MD, Somtochukwu Onwuzo, MD, Catherine Ly, MD, Ala Abdel Jalil, MD
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Brunner glands are exocrine glands found in duodenal mucosa and submucosa that secrete alkaline mucinous fluid, protecting the duodenal mucosa from the acidic stomach content. Brunner’s gland hyperplasia (BGH) is a rare benign tumor of the small intestine. It is often asymptomatic and usually incidentally detected during an EGD or imaging. In symptomatic patients, the most common presentations are gastrointestinal bleeding and gastric outlet obstruction. The majority of bleeding cases present with iron deficiency anemia.
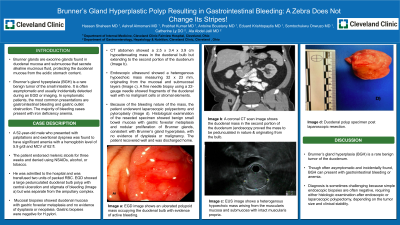
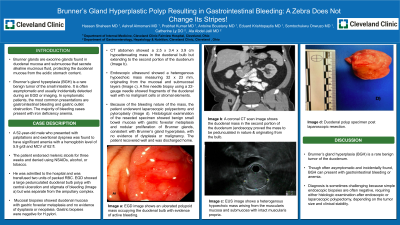
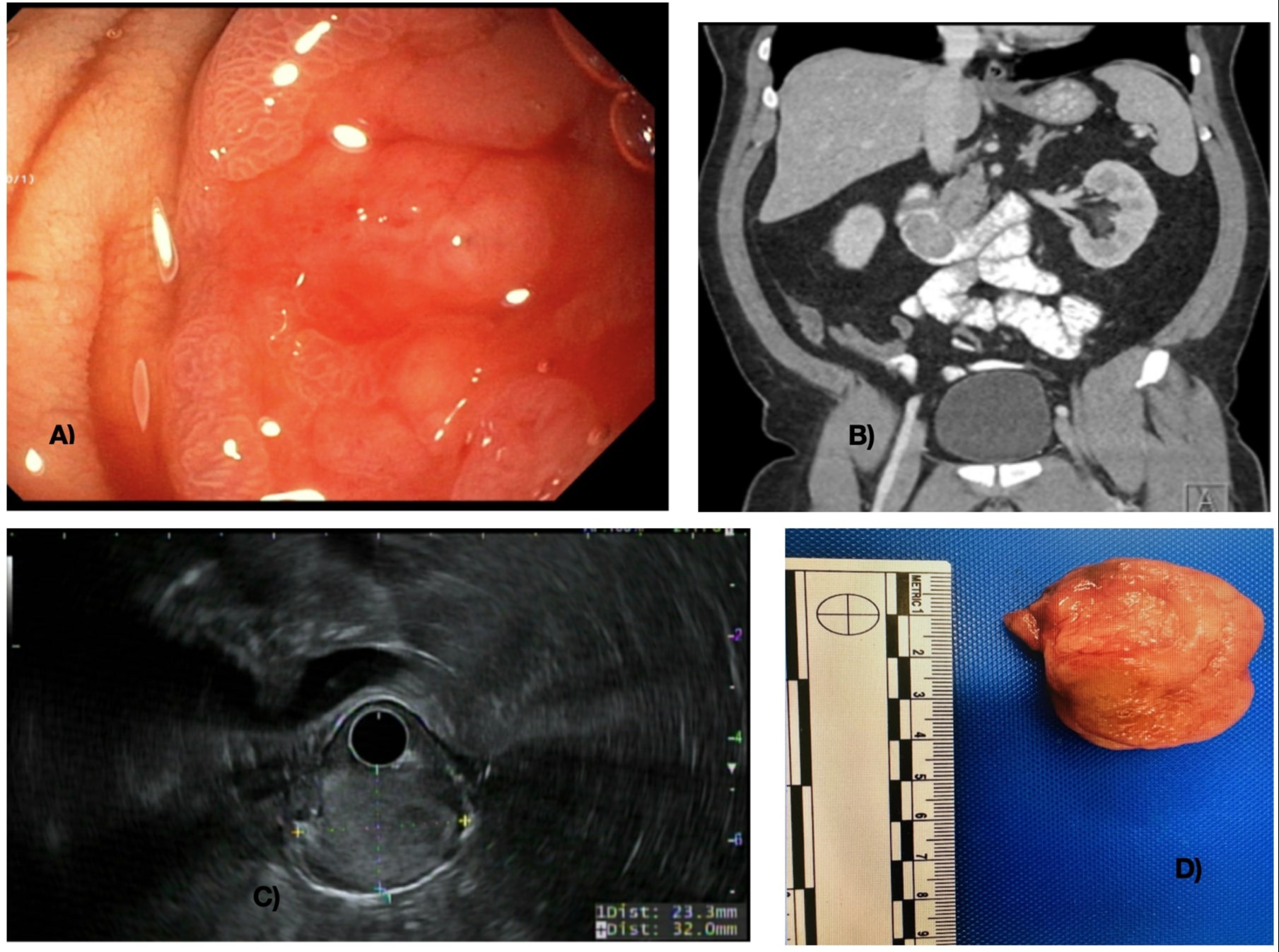
Case Description/Methods: A 52-year-old male who presented with palpitations and exertional dyspnea was found to have significant anemia with a hemoglobin level of 5.9 g/dl and MCV of 62 fl. The patient endorsed melenic stools for three weeks and denied using NSAIDs, alcohol, or tobacco. He was admitted to the hospital and was transfused two units of packed RBC. EGD showed a large pedunculated duodenal bulb polyp with central ulceration and stigmata of bleeding (Image a) but was separate from the ampullary complex. Mucosal biopsies showed duodenal mucosa with gastric foveolar metaplasia and no evidence of dysplasia or neoplasia. Gastric biopsies were negative for H.pylori. CT abdomen showed a 2.5 x 3.4 x 3.9 cm hypoattenuating mass in the duodenal bulb but extending to the second portion of the duodenum (Image b). Endoscopic ultrasound showed a heterogenous hypoechoic mass measuring 32 x 23 mm, originating from the mucosal and submucosal layers (Image c). A fine needle biopsy using a 22-gauge needle showed fragments of the duodenal wall with no malignant cells or stromal elements. Because of the bleeding nature of the mass, the patient underwent laparoscopic polypectomy and pyloroplasty (Image d). Histological examination of the resected specimen showed benign small bowel mucosa with gastric foveolar metaplasia and nodular proliferation of Brunner glands, consistent with Brunner’s gland hyperplasia, with no evidence of dysplasia or malignancy. The patient recovered well and was discharged home.
Discussion: Brunner’s gland hyperplasia (BGH) is a rare benign tumor of the duodenum. Though often asymptomatic and incidentally found, BGH can present with gastrointestinal bleeding or anemia. Diagnosis is sometimes challenging because simple endoscopic biopsies are often negative, requiring either histologic examination after endoscopic or laparoscopic polypectomy, depending on the tumor size and clinical stability.
Disclosures:
Hassan M. Shaheen, MD, Ashraf Almomani, MD, Prabhat Kumar, MD, Antoine Boustany, MD, MPH, Eduard Krishtopaytis, MD, Somtochukwu Onwuzo, MD, Catherine Ly, MD, Ala Abdel Jalil, MD. C0330 - Brunner’s Gland Hyperplastic Polyp Resulting in Gastrointestinal Bleeding: A Zebra Does Not Change Its Stripes!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Brunner glands are exocrine glands found in duodenal mucosa and submucosa that secrete alkaline mucinous fluid, protecting the duodenal mucosa from the acidic stomach content. Brunner’s gland hyperplasia (BGH) is a rare benign tumor of the small intestine. It is often asymptomatic and usually incidentally detected during an EGD or imaging. In symptomatic patients, the most common presentations are gastrointestinal bleeding and gastric outlet obstruction. The majority of bleeding cases present with iron deficiency anemia.
Case Description/Methods: A 52-year-old male who presented with palpitations and exertional dyspnea was found to have significant anemia with a hemoglobin level of 5.9 g/dl and MCV of 62 fl. The patient endorsed melenic stools for three weeks and denied using NSAIDs, alcohol, or tobacco. He was admitted to the hospital and was transfused two units of packed RBC. EGD showed a large pedunculated duodenal bulb polyp with central ulceration and stigmata of bleeding (Image a) but was separate from the ampullary complex. Mucosal biopsies showed duodenal mucosa with gastric foveolar metaplasia and no evidence of dysplasia or neoplasia. Gastric biopsies were negative for H.pylori. CT abdomen showed a 2.5 x 3.4 x 3.9 cm hypoattenuating mass in the duodenal bulb but extending to the second portion of the duodenum (Image b). Endoscopic ultrasound showed a heterogenous hypoechoic mass measuring 32 x 23 mm, originating from the mucosal and submucosal layers (Image c). A fine needle biopsy using a 22-gauge needle showed fragments of the duodenal wall with no malignant cells or stromal elements. Because of the bleeding nature of the mass, the patient underwent laparoscopic polypectomy and pyloroplasty (Image d). Histological examination of the resected specimen showed benign small bowel mucosa with gastric foveolar metaplasia and nodular proliferation of Brunner glands, consistent with Brunner’s gland hyperplasia, with no evidence of dysplasia or malignancy. The patient recovered well and was discharged home.
Discussion: Brunner’s gland hyperplasia (BGH) is a rare benign tumor of the duodenum. Though often asymptomatic and incidentally found, BGH can present with gastrointestinal bleeding or anemia. Diagnosis is sometimes challenging because simple endoscopic biopsies are often negative, requiring either histologic examination after endoscopic or laparoscopic polypectomy, depending on the tumor size and clinical stability.
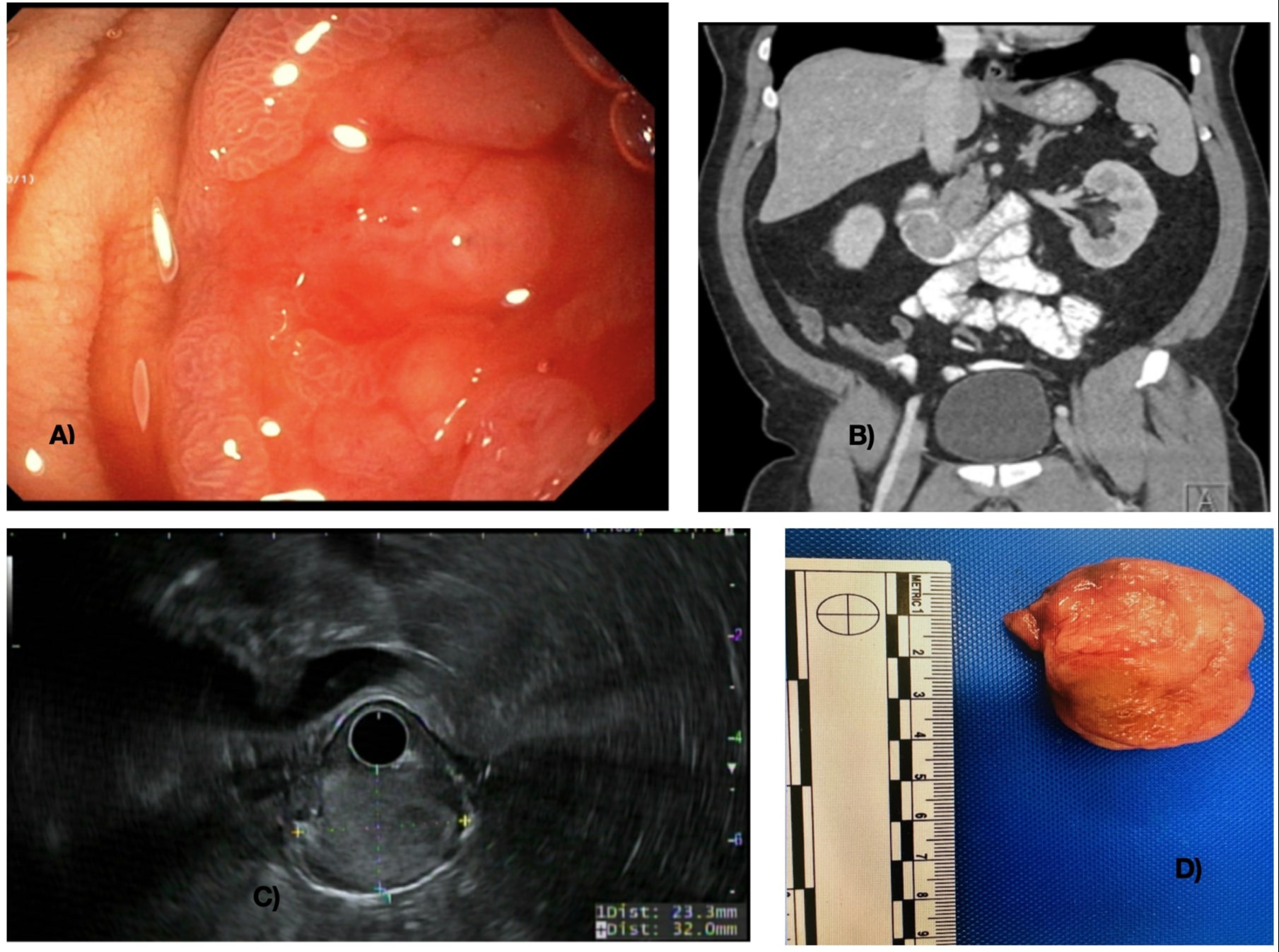
Figure: a) EGD image shows an ulcerated polypoid mass occupying the duodenal bulb with evidence of active bleeding. b) A coronal CT scan image shows the duodenal mass in the second portion of the duodenum (endoscopy proved the mass to be pedunculated in nature & originating from the bulb. c) EUS image shows a heterogenous hypoechoic mass arising from the muscularis mucosa and submucosa with intact muscularis propria. d) Duodenal polyp specimen post laparoscopic resection.
Disclosures:
Hassan Shaheen indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Eduard Krishtopaytis indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Catherine Ly indicated no relevant financial relationships.
Ala Abdel Jalil indicated no relevant financial relationships.
Hassan M. Shaheen, MD, Ashraf Almomani, MD, Prabhat Kumar, MD, Antoine Boustany, MD, MPH, Eduard Krishtopaytis, MD, Somtochukwu Onwuzo, MD, Catherine Ly, MD, Ala Abdel Jalil, MD. C0330 - Brunner’s Gland Hyperplastic Polyp Resulting in Gastrointestinal Bleeding: A Zebra Does Not Change Its Stripes!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
