Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0429 - Diagnosing Visceral Kaposi Sarcoma: The Necessity to Avoid Anchoring on the Diagnosis of a Crohn's Flare
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Emily Seltzer, DO, MS
Icahn School of Medicine at Mount Sinai Morningside-West
New York, NY
Presenting Author(s)
Emily Seltzer, DO, MS, Shabari M. Shenoy, MBBS, Bo Hyung Yoon, MD, Frederick Rozenshteyn, MD, Kevin Mijares, MD, Kimberly Cavaliere, MD
Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY
Introduction: Inflammatory bowel disease (IBD) and human immunodeficiency virus (HIV) affect the immune system in inverse means, IBD causes an overdrive of the immune system whereas HIV suppresses it. The decline in CD4+ count in HIV is believed to promote remission of IBD by decreasing inflammatory responses.
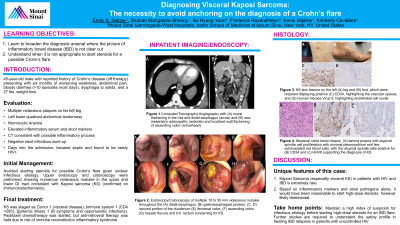
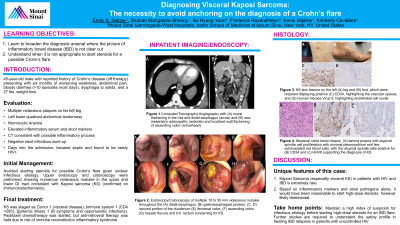
Case Description/Methods: We present a 45-year-old male with a self-reported history of Crohn’s disease (CD) complaining of bloody diarrhea and weight loss that he presumed to be the result of a Crohn’s flair. He was afebrile and tachycardic with multiple violaceous plaques on his left leg and left lower quadrant abdominal tenderness on exam. Labs were significant for anemia, elevated C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin. Abdominal computed tomography angiography revealed mild mural thickening in the mid to distal esophagus, mesenteric adenopathy, and wall thickening of the ascending colon. To rule out infectious causes, Clostridium difficile and gastrointestinal pathogens panel were collected and resulted as negative. The patient’s course was complicated by sepsis of unknown etiology. Further investigation revealed his lower extremity lesions were recently biopsied establishing a diagnosis of Kaposi Sarcoma (KS). Initiation of high-dose glucocorticoids for possible Crohn’s flare was deferred in light of this. Despite previous negative results, HIV antigen was positive with a CD4+ count of 58 cells/mm3 and viral load >1,000,000 copies/mL. Upper endoscopy and colonoscopy demonstrated many 10 to 50 mm violaceous nodules in the esophagus, duodenum, and throughout the colon consistent with KS. This was confirmed immunohistochemistry positive for CD34 and HHV8. The KS was staged as Tumor 1 (visceral disease), Immune system 1 (CD4< 200), Systemic illness 1 (B symptoms). He was started on paclitaxel, with anti-retroviral therapy held due to increased risk of immune reconstitution inflammatory syndrome.
Discussion: KS in patients with HIV and IBD is extremely rare with a prevalence of 0.4%, and, visceral KS is rarely present with initial diagnosis of HIV. We demonstrate the risks of anchoring on a CD diagnosis of CD, as it is possible HIV would have been missed and starting treatment of CD could have been very harmful as high-dose steroids have been shown to further progress KS. We share this truly rare case of visceral KS in a patient with newly diagnosed HIV masquerading as a CD flare to promote broadening the diagnostic arsenal where the picture of IBD is not clear cut.
Disclosures:
Emily Seltzer, DO, MS, Shabari M. Shenoy, MBBS, Bo Hyung Yoon, MD, Frederick Rozenshteyn, MD, Kevin Mijares, MD, Kimberly Cavaliere, MD. E0429 - Diagnosing Visceral Kaposi Sarcoma: The Necessity to Avoid Anchoring on the Diagnosis of a Crohn's Flare, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY
Introduction: Inflammatory bowel disease (IBD) and human immunodeficiency virus (HIV) affect the immune system in inverse means, IBD causes an overdrive of the immune system whereas HIV suppresses it. The decline in CD4+ count in HIV is believed to promote remission of IBD by decreasing inflammatory responses.
Case Description/Methods: We present a 45-year-old male with a self-reported history of Crohn’s disease (CD) complaining of bloody diarrhea and weight loss that he presumed to be the result of a Crohn’s flair. He was afebrile and tachycardic with multiple violaceous plaques on his left leg and left lower quadrant abdominal tenderness on exam. Labs were significant for anemia, elevated C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin. Abdominal computed tomography angiography revealed mild mural thickening in the mid to distal esophagus, mesenteric adenopathy, and wall thickening of the ascending colon. To rule out infectious causes, Clostridium difficile and gastrointestinal pathogens panel were collected and resulted as negative. The patient’s course was complicated by sepsis of unknown etiology. Further investigation revealed his lower extremity lesions were recently biopsied establishing a diagnosis of Kaposi Sarcoma (KS). Initiation of high-dose glucocorticoids for possible Crohn’s flare was deferred in light of this. Despite previous negative results, HIV antigen was positive with a CD4+ count of 58 cells/mm3 and viral load >1,000,000 copies/mL. Upper endoscopy and colonoscopy demonstrated many 10 to 50 mm violaceous nodules in the esophagus, duodenum, and throughout the colon consistent with KS. This was confirmed immunohistochemistry positive for CD34 and HHV8. The KS was staged as Tumor 1 (visceral disease), Immune system 1 (CD4< 200), Systemic illness 1 (B symptoms). He was started on paclitaxel, with anti-retroviral therapy held due to increased risk of immune reconstitution inflammatory syndrome.
Discussion: KS in patients with HIV and IBD is extremely rare with a prevalence of 0.4%, and, visceral KS is rarely present with initial diagnosis of HIV. We demonstrate the risks of anchoring on a CD diagnosis of CD, as it is possible HIV would have been missed and starting treatment of CD could have been very harmful as high-dose steroids have been shown to further progress KS. We share this truly rare case of visceral KS in a patient with newly diagnosed HIV masquerading as a CD flare to promote broadening the diagnostic arsenal where the picture of IBD is not clear cut.
Disclosures:
Emily Seltzer indicated no relevant financial relationships.
Shabari Shenoy indicated no relevant financial relationships.
Bo Hyung Yoon indicated no relevant financial relationships.
Frederick Rozenshteyn indicated no relevant financial relationships.
Kevin Mijares indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Emily Seltzer, DO, MS, Shabari M. Shenoy, MBBS, Bo Hyung Yoon, MD, Frederick Rozenshteyn, MD, Kevin Mijares, MD, Kimberly Cavaliere, MD. E0429 - Diagnosing Visceral Kaposi Sarcoma: The Necessity to Avoid Anchoring on the Diagnosis of a Crohn's Flare, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
