Back

Poster Session E - Tuesday Afternoon
Category: Interventional Endoscopy
E0444 - Stenting as Salvage Therapy for Colonic Perforation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- AB
Aaron Brenner, MD
University of Kentucky College of Medicine
Lexington, KY
Presenting Author(s)
Aaron Brenner, MD1, Nimish Thakral, MD2, Samuel Mardini, MD, MBA, MPH, FACG2
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: The presence of Cirrhosis in perforated diverticular disease can amplify mortality several-fold. Ascites and abdominal venous collaterals can limit operative intervention. The absence of meaningful data limits rescue therapy in such cases. We present a unique case of colonic stent placement as a rescue attempt in a patient with decompensated cirrhosis and perforated diverticular disease.
Case Description/Methods: A 62-year-old female with a history of alcohol-related cirrhosis decompensated by variceal bleeding presented with 3 days of diffuse abdominal pain and abdominal distention. CT scan revealed a contained micro-perforation in the sigmoid colon along with new onset ascites. Paracentesis done on admission was indicative of underlying secondary bacterial peritonitis (ScBP) and the patient was started on antimicrobial therapy. Colorectal surgery evaluated the patient and recommended conservative management in the setting of a contained micro-perforation. The patient's course was complicated by frank perforation and septic shock. the patient was deemed not to be a surgical candidate given high intra-operative mortality in the setting of Child Pugh Category C Cirrhosis. Shock physiology resolved with antimicrobial therapy and TPN, but the patient continued to have ScBP on repeat paracentesis. Given the patient’s good functional status prior to the admission, rescue therapy was attempted.
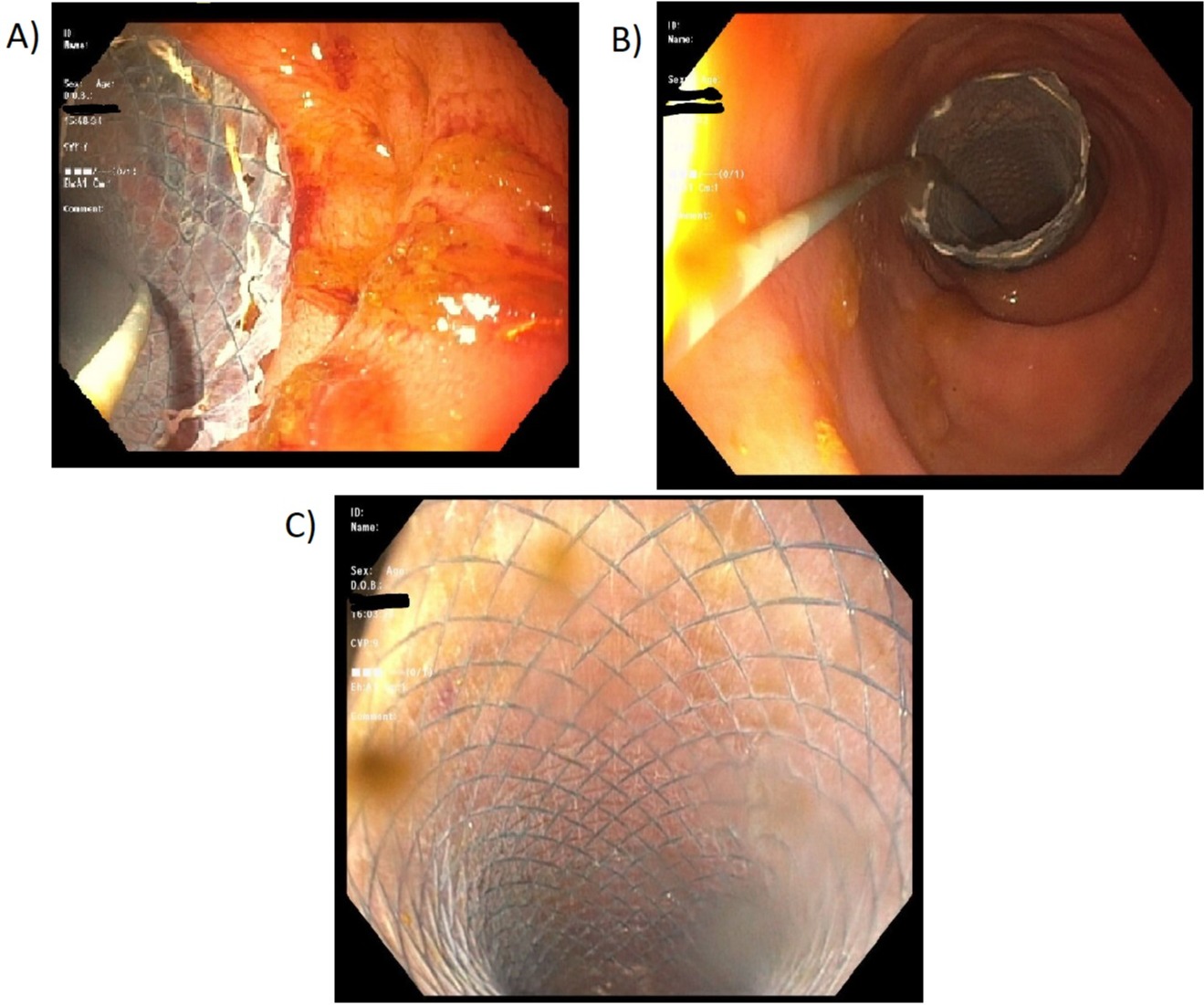
Three 20 mm wide, 15 cm long fully covered stents were placed endoscopically in an overlapping fashion starting 10cm proximal to the presumed site of perforation and extended to the rectum. A total of 40-45 cm in length was covered. The proximal and distal stents were each anchored with three 16mm Duraclips. Subsequently, there was a decrease in ascitic fluid neutrophil count from 7,614uL to 2,116uL. However, one of the stents dislodged on day 3 post procedure and the ascitic fluid neutrophil count increased to 10,000uL again. Unfortunately, the patient developed variceal bleeding a week later and the family decided to proceed with comfort care measures.
Discussion: Colonic perforation is a dreaded complication of diverticular disease with an annual incidence of 4/100,0000. The associated mortality in patients undergoing an operative intervention is estimated at 12% to 36%. The presence of underlying cirrhosis and ascites can amplify mortality many-fold. In such conditions, when a surgical approach is contraindicated, endoluminal salvage therapy with colonic stents to bypass the perforation can be attempted.
Disclosures:
Aaron Brenner, MD1, Nimish Thakral, MD2, Samuel Mardini, MD, MBA, MPH, FACG2. E0444 - Stenting as Salvage Therapy for Colonic Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky College of Medicine, Lexington, KY; 2University of Kentucky, Lexington, KY
Introduction: The presence of Cirrhosis in perforated diverticular disease can amplify mortality several-fold. Ascites and abdominal venous collaterals can limit operative intervention. The absence of meaningful data limits rescue therapy in such cases. We present a unique case of colonic stent placement as a rescue attempt in a patient with decompensated cirrhosis and perforated diverticular disease.
Case Description/Methods: A 62-year-old female with a history of alcohol-related cirrhosis decompensated by variceal bleeding presented with 3 days of diffuse abdominal pain and abdominal distention. CT scan revealed a contained micro-perforation in the sigmoid colon along with new onset ascites. Paracentesis done on admission was indicative of underlying secondary bacterial peritonitis (ScBP) and the patient was started on antimicrobial therapy. Colorectal surgery evaluated the patient and recommended conservative management in the setting of a contained micro-perforation. The patient's course was complicated by frank perforation and septic shock. the patient was deemed not to be a surgical candidate given high intra-operative mortality in the setting of Child Pugh Category C Cirrhosis. Shock physiology resolved with antimicrobial therapy and TPN, but the patient continued to have ScBP on repeat paracentesis. Given the patient’s good functional status prior to the admission, rescue therapy was attempted.
Three 20 mm wide, 15 cm long fully covered stents were placed endoscopically in an overlapping fashion starting 10cm proximal to the presumed site of perforation and extended to the rectum. A total of 40-45 cm in length was covered. The proximal and distal stents were each anchored with three 16mm Duraclips. Subsequently, there was a decrease in ascitic fluid neutrophil count from 7,614uL to 2,116uL. However, one of the stents dislodged on day 3 post procedure and the ascitic fluid neutrophil count increased to 10,000uL again. Unfortunately, the patient developed variceal bleeding a week later and the family decided to proceed with comfort care measures.
Discussion: Colonic perforation is a dreaded complication of diverticular disease with an annual incidence of 4/100,0000. The associated mortality in patients undergoing an operative intervention is estimated at 12% to 36%. The presence of underlying cirrhosis and ascites can amplify mortality many-fold. In such conditions, when a surgical approach is contraindicated, endoluminal salvage therapy with colonic stents to bypass the perforation can be attempted.
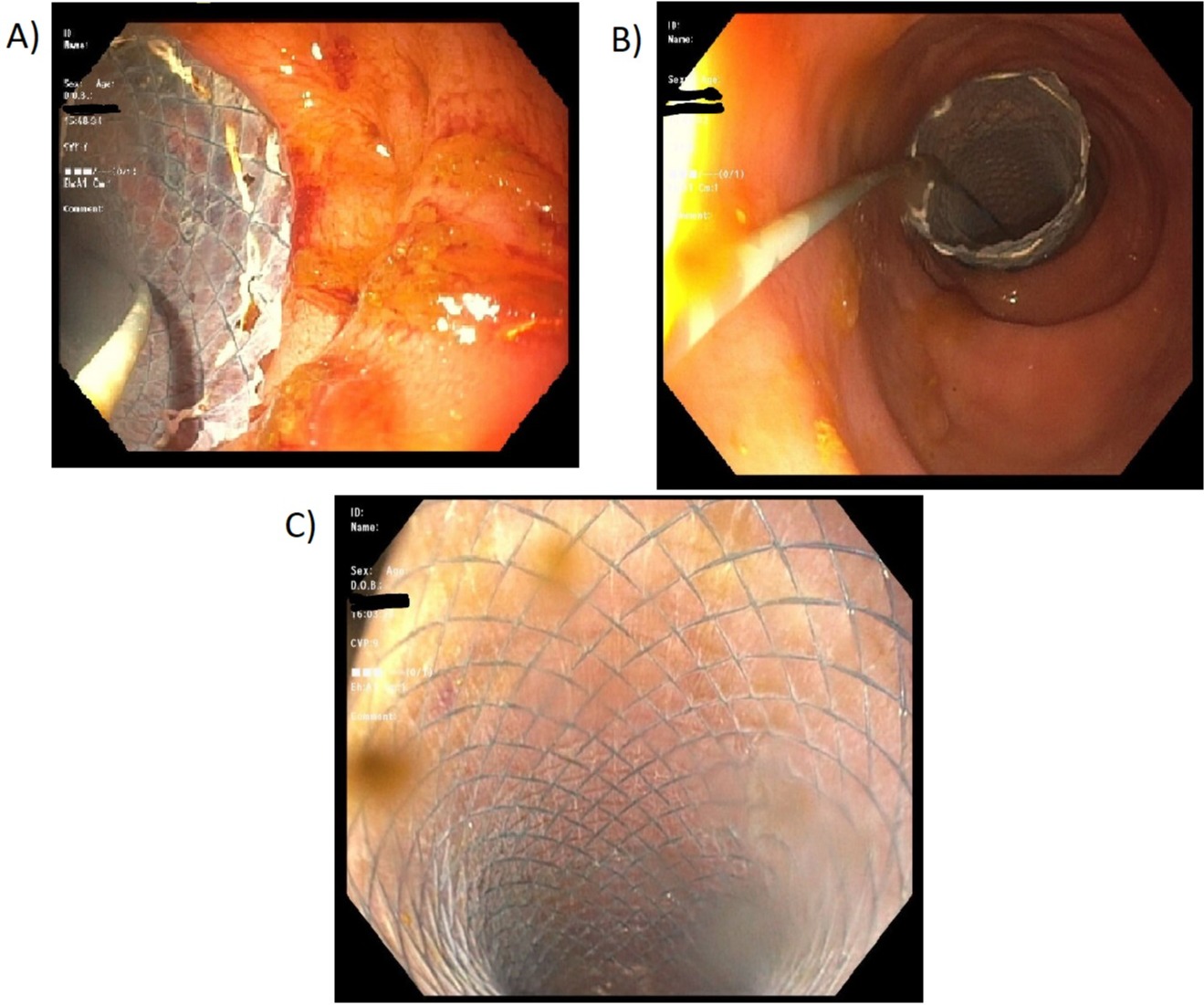
Figure: Image 1: A and B) Stent placement in sigmoid colon. C) Patent stent with free flowing stool through the stent.
Disclosures:
Aaron Brenner indicated no relevant financial relationships.
Nimish Thakral indicated no relevant financial relationships.
Samuel Mardini indicated no relevant financial relationships.
Aaron Brenner, MD1, Nimish Thakral, MD2, Samuel Mardini, MD, MBA, MPH, FACG2. E0444 - Stenting as Salvage Therapy for Colonic Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
