Back

Poster Session E - Tuesday Afternoon
Category: Interventional Endoscopy
E0451 - Mucosal Ablation Salvage Therapy After Prior TIF for Recurrent GERD
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Luke Kennedy, MD
Baylor College of Medicine
Bellaire, TX
Presenting Author(s)
Award: Presidential Poster Award
Luke Kennedy, MD, Peter Nguyen, MD, Jordan Sparkman, MD, Kalpesh K. Patel, MD
Baylor College of Medicine, Houston, TX
Introduction: Gastroesophageal reflux disease (GERD) is a major cause of upper GI complaints and affects approximately a quarter of Americans. If medical therapy with proton pump inhibitors or histamine antagonists fails, there are endoscopic interventions that can be offered to decrease symptoms. One such endoscopic procedure is called anti-reflux mucosal ablation or ARMA. ARMA is a minimally invasive option available to the general endoscopist even in low resource settings and can be an effective treatment even after other techniques have been attempted such as transoral incisionless fundoplication (TIF).
Case Description/Methods: A 66-year-old female with severe GERD, confirmed with pH impedance testing, presented with recurrent heartburn two years after successful treatment with TIF. High dose PPI improved the pain but did not resolve it. She continued to have daily severe symptoms. She could not identify any dietary triggers or exacerbating factors other than laying down or bending over. She had no hematemesis, dysphagia or abdominal pain. There was no family history of esophageal or gastric cancer.
After discussion of her therapeutic options, she chose to pursue endoscopy with anti-reflux mucosal ablation (ARMA). The patient’s GERD quality of life questionnaire was obtained at 0, 3 and 6-month follow-up from ARMA. The questionnaire consists of 10 questions on a scale of 1-5 with highest numbers being the most severe symptoms related to GERD. Her scoring improved from an initial score of 33 (max 50) down to 13 then 7 at 0, 3, and 6-month follow-up, respectively.
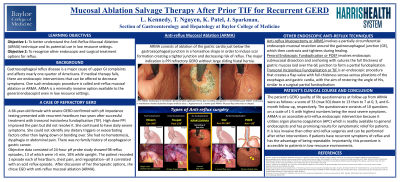
Discussion: ARMA consists of ablation of the gastric mucosa in a horseshoe shape around the lower esophageal sphincter to induce scar tissue formation. As it contracts, it creates a tighter junction and decreases the risk of reflux. (See picture below). Circumferential ablation is avoided to decrease the risk for strictures. ARMA is an accessible anti-reflux endoscopic intervention because it utilizes argon plasma coagulation (APC) which is readily available to general endoscopists and has promising results for symptomatic relief for patients. It is less invasive than other anti-reflux surgeries and can be performed after other interventions if patients have recurrent symptoms of reflux and has the advantage of being repeatable. Importantly, this procedure is accessible to patients in low-resource environments, such as our county health system.

Disclosures:
Luke Kennedy, MD, Peter Nguyen, MD, Jordan Sparkman, MD, Kalpesh K. Patel, MD. E0451 - Mucosal Ablation Salvage Therapy After Prior TIF for Recurrent GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Luke Kennedy, MD, Peter Nguyen, MD, Jordan Sparkman, MD, Kalpesh K. Patel, MD
Baylor College of Medicine, Houston, TX
Introduction: Gastroesophageal reflux disease (GERD) is a major cause of upper GI complaints and affects approximately a quarter of Americans. If medical therapy with proton pump inhibitors or histamine antagonists fails, there are endoscopic interventions that can be offered to decrease symptoms. One such endoscopic procedure is called anti-reflux mucosal ablation or ARMA. ARMA is a minimally invasive option available to the general endoscopist even in low resource settings and can be an effective treatment even after other techniques have been attempted such as transoral incisionless fundoplication (TIF).
Case Description/Methods: A 66-year-old female with severe GERD, confirmed with pH impedance testing, presented with recurrent heartburn two years after successful treatment with TIF. High dose PPI improved the pain but did not resolve it. She continued to have daily severe symptoms. She could not identify any dietary triggers or exacerbating factors other than laying down or bending over. She had no hematemesis, dysphagia or abdominal pain. There was no family history of esophageal or gastric cancer.
After discussion of her therapeutic options, she chose to pursue endoscopy with anti-reflux mucosal ablation (ARMA). The patient’s GERD quality of life questionnaire was obtained at 0, 3 and 6-month follow-up from ARMA. The questionnaire consists of 10 questions on a scale of 1-5 with highest numbers being the most severe symptoms related to GERD. Her scoring improved from an initial score of 33 (max 50) down to 13 then 7 at 0, 3, and 6-month follow-up, respectively.
Discussion: ARMA consists of ablation of the gastric mucosa in a horseshoe shape around the lower esophageal sphincter to induce scar tissue formation. As it contracts, it creates a tighter junction and decreases the risk of reflux. (See picture below). Circumferential ablation is avoided to decrease the risk for strictures. ARMA is an accessible anti-reflux endoscopic intervention because it utilizes argon plasma coagulation (APC) which is readily available to general endoscopists and has promising results for symptomatic relief for patients. It is less invasive than other anti-reflux surgeries and can be performed after other interventions if patients have recurrent symptoms of reflux and has the advantage of being repeatable. Importantly, this procedure is accessible to patients in low-resource environments, such as our county health system.

Figure: Example of Endoscopic View: a Pre-ARMA. Endoscopy in retroflexion demonstrated significant hernia but no sliding component. b Immediately post-ARMA. Endoscopy in retroflexion showed horseshoe-shaped artificial ulcer. c Appearance at 1 month post-ARMA. Mucosal flap valve was re-shaped.
Inoue H et al. Anti-reflux mucosal ablation (ARMA) as a new treatment for gastroesophageal reflux refractory to proton pump inhibitors: a pilot study. Endosc Int Open. 2020 Feb;8
Inoue H et al. Anti-reflux mucosal ablation (ARMA) as a new treatment for gastroesophageal reflux refractory to proton pump inhibitors: a pilot study. Endosc Int Open. 2020 Feb;8
Disclosures:
Luke Kennedy indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Jordan Sparkman indicated no relevant financial relationships.
Kalpesh Patel: Boston Scientific – Consultant.
Luke Kennedy, MD, Peter Nguyen, MD, Jordan Sparkman, MD, Kalpesh K. Patel, MD. E0451 - Mucosal Ablation Salvage Therapy After Prior TIF for Recurrent GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

