Back

Poster Session E - Tuesday Afternoon
Category: Interventional Endoscopy
E0455 - Hidden in Plain Sight: Cholangiocarcinoma Diagnosed With Laparoscopy After Multiple Non-Diagnostic ERCPs
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Peter M. Stawinski, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Peter M. Stawinski, MD, Karolina N. Dziadkowiec, MD, Nichole Henkes, , Natasha McMillan, MD, Laura Rosenkranz, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Cholangiocarcinoma (CCA) is a malignancy of the biliary tree, composed of epithelial cells and presents insidiously. Endoscopic retrograde cholangiopancreatography (ERCP) is used in the diagnosis and treatment of biliary strictures and malignant biliary obstruction.
Case Description/Methods: A 42-year-old man with a 9-month history of cholestatic-pattern of liver test elevation who presented for evaluation of abnormal liver tests, persistent pruritus, intermittent abdominal pain. Social history was negative for toxic habits.
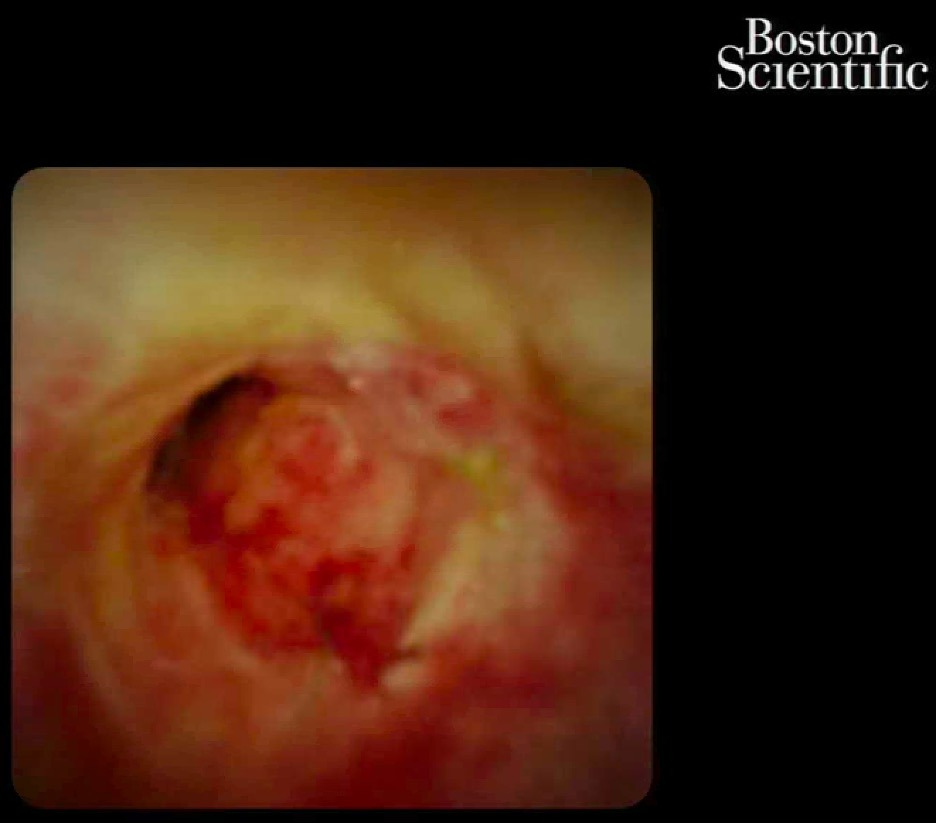
Prior to presentation, the patient was being treated for presumed drug-induced liver injury (DILI) with a cholestatic pattern of liver injury. On admission, the patient's vital signs were within normal limits. Physical examination was significant for generalized pruritus, jaundice, and right upper quadrant abdominal pain and negative for signs of chronic liver disease. Liver biopsy revealed ductular proliferation with periportal fibrosis and a neutrophil-rich portal infiltrate suggestive of a large duct obstruction. Magnetic resonance cholangiopancreatography (MRCP) revealed a high-grade stricture involving the common hepatic duct (CHD) with intrahepatic duct dilation. An initial ERCP with SpyGlass was performed with visualization of the CHD stricture, which was dilated, biopsied and stented. Biopsy results revealed intestinal metaplasia. A repeat ERCP was completed due to continued abdominal pain and revealed a 40 mm stricture in the CHD with the mucosa appearing friable, ulcerated, and nodular with masses suspicious for CCA. Biopsy resulted in inflammation without malignancy. Repeat ERCP and endoscopic ultrasound (EUS) revealed prior CHD stricture, an irregular, spiculated mass in the CHD. Biopsy results revealed benign epithelium. He was referred for surgical evaluation but surgery was deferred due to multiple benign tissue samples and the risk of surgery. He was ultimately discharged and underwent an exploratory laparotomy in Houston and was found to have CCA.
Discussion: CCA is the second most common primary hepatic malignancy. Imaging can assist in the identification of CCA, but confirmation is with tissue biopsy. Tissue is obtained through endoscopic means or open surgical resection. In this case, multiple ERCP-guided biopsies revealed benign tissue, but found to have CCA after exploratory laparotomy. When diagnostic imaging and procedures fail to establish a diagnosis, the physician must rely on their own expertise and knowledge to identify the underlying cause.
Disclosures:
Peter M. Stawinski, MD, Karolina N. Dziadkowiec, MD, Nichole Henkes, , Natasha McMillan, MD, Laura Rosenkranz, MD. E0455 - Hidden in Plain Sight: Cholangiocarcinoma Diagnosed With Laparoscopy After Multiple Non-Diagnostic ERCPs, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Cholangiocarcinoma (CCA) is a malignancy of the biliary tree, composed of epithelial cells and presents insidiously. Endoscopic retrograde cholangiopancreatography (ERCP) is used in the diagnosis and treatment of biliary strictures and malignant biliary obstruction.
Case Description/Methods: A 42-year-old man with a 9-month history of cholestatic-pattern of liver test elevation who presented for evaluation of abnormal liver tests, persistent pruritus, intermittent abdominal pain. Social history was negative for toxic habits.
Prior to presentation, the patient was being treated for presumed drug-induced liver injury (DILI) with a cholestatic pattern of liver injury. On admission, the patient's vital signs were within normal limits. Physical examination was significant for generalized pruritus, jaundice, and right upper quadrant abdominal pain and negative for signs of chronic liver disease. Liver biopsy revealed ductular proliferation with periportal fibrosis and a neutrophil-rich portal infiltrate suggestive of a large duct obstruction. Magnetic resonance cholangiopancreatography (MRCP) revealed a high-grade stricture involving the common hepatic duct (CHD) with intrahepatic duct dilation. An initial ERCP with SpyGlass was performed with visualization of the CHD stricture, which was dilated, biopsied and stented. Biopsy results revealed intestinal metaplasia. A repeat ERCP was completed due to continued abdominal pain and revealed a 40 mm stricture in the CHD with the mucosa appearing friable, ulcerated, and nodular with masses suspicious for CCA. Biopsy resulted in inflammation without malignancy. Repeat ERCP and endoscopic ultrasound (EUS) revealed prior CHD stricture, an irregular, spiculated mass in the CHD. Biopsy results revealed benign epithelium. He was referred for surgical evaluation but surgery was deferred due to multiple benign tissue samples and the risk of surgery. He was ultimately discharged and underwent an exploratory laparotomy in Houston and was found to have CCA.
Discussion: CCA is the second most common primary hepatic malignancy. Imaging can assist in the identification of CCA, but confirmation is with tissue biopsy. Tissue is obtained through endoscopic means or open surgical resection. In this case, multiple ERCP-guided biopsies revealed benign tissue, but found to have CCA after exploratory laparotomy. When diagnostic imaging and procedures fail to establish a diagnosis, the physician must rely on their own expertise and knowledge to identify the underlying cause.
Figure: Deeply ulcerated, friable and strictured mucosa identified via SpyGlass in the common hepatic duct.
Disclosures:
Peter Stawinski indicated no relevant financial relationships.
Karolina Dziadkowiec indicated no relevant financial relationships.
Nichole Henkes indicated no relevant financial relationships.
Natasha McMillan indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Peter M. Stawinski, MD, Karolina N. Dziadkowiec, MD, Nichole Henkes, , Natasha McMillan, MD, Laura Rosenkranz, MD. E0455 - Hidden in Plain Sight: Cholangiocarcinoma Diagnosed With Laparoscopy After Multiple Non-Diagnostic ERCPs, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
