Back

Poster Session B - Monday Morning
Category: IBD
B0421 - Case Report: Mycobacterium paragordonae Associated Crohn's Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Yuntao Zou, MD
Saint Peter's University Hospital
New Brunswick, NJ
Presenting Author(s)
Yuntao Zou, MD1, Yi-Chia Wu, MD2, Andrew Korman, MD2
1Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: We are reporting a case of Mycobacterium Paragordonae (M. Paragordonae) related to Crohn's disease (CD).
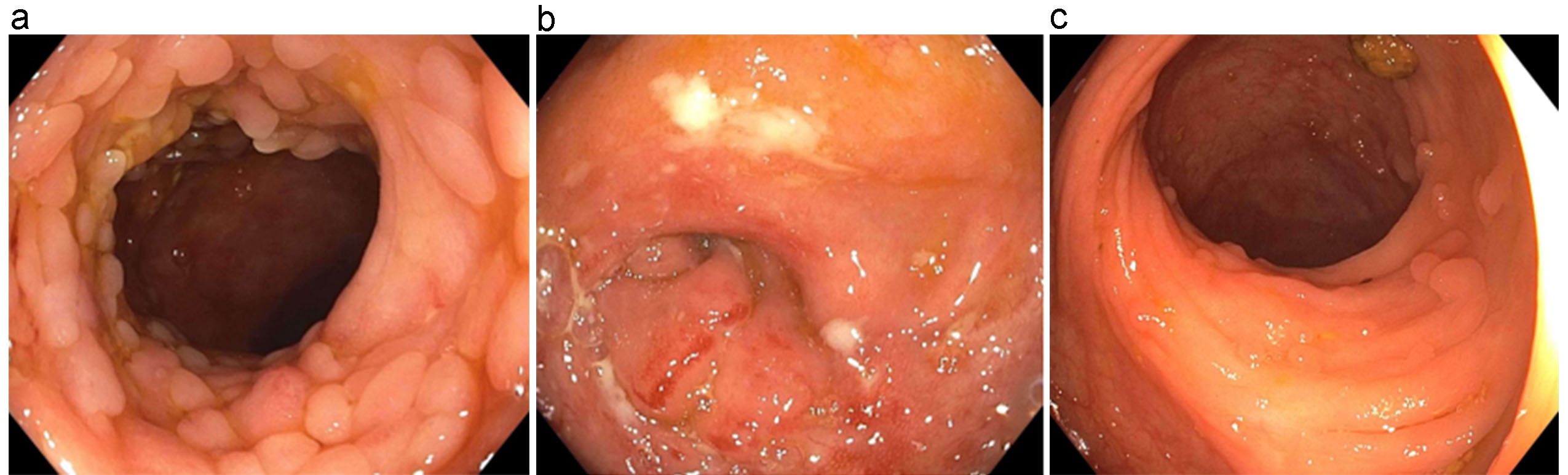
Case Description/Methods: A 44-year-old man presented with right-sided abdominal pain and non-bloody diarrhea. No weight loss or fevers. Labs were significant for calprotectin 117 ug/g and negative infectious stool studies. CT scan showed thickening of the ascending colon. Colonoscopy demonstrated ulcerated mucosa with pseudopolyps from the cecum to the hepatic flexure with pathology of crypt abscesses and poorly formed noncaseating granulomas, which was consistent with Crohn's colitis (Fig. a & b). Capsule endoscopy was negative for small bowel disease. While waiting to start biologics, mesalamine was started. A repeat colonoscopy 6 months afterwards continued to show right-sided colitis. Meanwhile, the QuantiFERON-TB gold test was found to be positive. Chest X-ray showed fibronodular changes within the lung apices bilaterally. Sputum acid-fast smear was negative, but culture was positive. Further identification showed M. Paragordonae. While pending the final speciation of mycobacterium, treatment with 4-drug RIPE treatment was initiated for concern of possible active tuberculosis. The patient refused to continue the full RIPE treatment due to side effects. Therefore, it was decided to continue isoniazid and rifampin daily for another 5 months. The patient’s symptoms improved significantly. Repeat colonoscopy after treatment showed markedly improved colitis (Fig. c).
Discussion: The relationship between CD and mycobacterium species needs further elucidation. Both CD and tuberculosis (TB) can cause granulomatous inflammation of the GI tract, which can be difficult to distinguish. Although histopathologically similar, caseating granulomas are seen in TB. It has also been suggested Mycobacterium avium subspecies paratuberculosis (MAP) as an etiology for CD since it is more prevalent in CD patients. Reports of these patients have shown remission after mycobacterial treatment. Although the histopathology of our patient is consistent with CD, there was significant improvement after mycobacterial treatment. Although M. Paragordonae is a nontuberculosis species, it is unclear if this may reflect the variability of culture sensitivity in detecting TB or a new mycobacterium associated with CD, as previously seen with MAP. Nonetheless, this case emphasizes the importance of having a high suspicion for TB in suspected CD. If identified correctly, these patients can be promptly started on treatment.
Disclosures:
Yuntao Zou, MD1, Yi-Chia Wu, MD2, Andrew Korman, MD2. B0421 - Case Report: Mycobacterium paragordonae Associated Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: We are reporting a case of Mycobacterium Paragordonae (M. Paragordonae) related to Crohn's disease (CD).
Case Description/Methods: A 44-year-old man presented with right-sided abdominal pain and non-bloody diarrhea. No weight loss or fevers. Labs were significant for calprotectin 117 ug/g and negative infectious stool studies. CT scan showed thickening of the ascending colon. Colonoscopy demonstrated ulcerated mucosa with pseudopolyps from the cecum to the hepatic flexure with pathology of crypt abscesses and poorly formed noncaseating granulomas, which was consistent with Crohn's colitis (Fig. a & b). Capsule endoscopy was negative for small bowel disease. While waiting to start biologics, mesalamine was started. A repeat colonoscopy 6 months afterwards continued to show right-sided colitis. Meanwhile, the QuantiFERON-TB gold test was found to be positive. Chest X-ray showed fibronodular changes within the lung apices bilaterally. Sputum acid-fast smear was negative, but culture was positive. Further identification showed M. Paragordonae. While pending the final speciation of mycobacterium, treatment with 4-drug RIPE treatment was initiated for concern of possible active tuberculosis. The patient refused to continue the full RIPE treatment due to side effects. Therefore, it was decided to continue isoniazid and rifampin daily for another 5 months. The patient’s symptoms improved significantly. Repeat colonoscopy after treatment showed markedly improved colitis (Fig. c).
Discussion: The relationship between CD and mycobacterium species needs further elucidation. Both CD and tuberculosis (TB) can cause granulomatous inflammation of the GI tract, which can be difficult to distinguish. Although histopathologically similar, caseating granulomas are seen in TB. It has also been suggested Mycobacterium avium subspecies paratuberculosis (MAP) as an etiology for CD since it is more prevalent in CD patients. Reports of these patients have shown remission after mycobacterial treatment. Although the histopathology of our patient is consistent with CD, there was significant improvement after mycobacterial treatment. Although M. Paragordonae is a nontuberculosis species, it is unclear if this may reflect the variability of culture sensitivity in detecting TB or a new mycobacterium associated with CD, as previously seen with MAP. Nonetheless, this case emphasizes the importance of having a high suspicion for TB in suspected CD. If identified correctly, these patients can be promptly started on treatment.
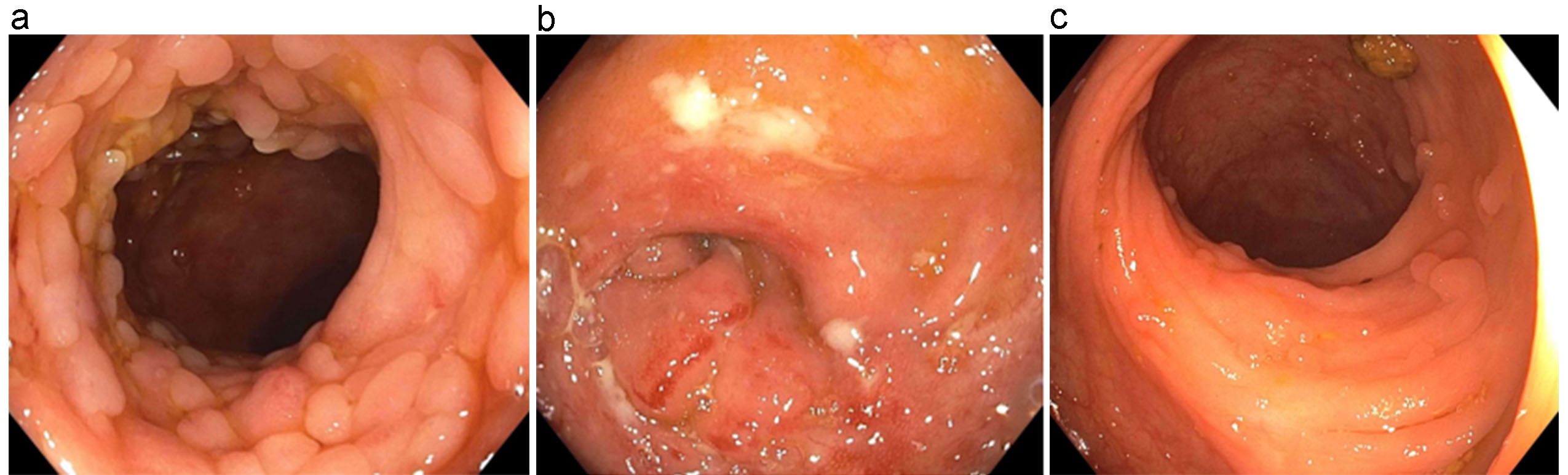
Figure: Colonoscopy on inital presentation( a & b) and after RIPE treament (c)
Disclosures:
Yuntao Zou indicated no relevant financial relationships.
Yi-Chia Wu indicated no relevant financial relationships.
Andrew Korman indicated no relevant financial relationships.
Yuntao Zou, MD1, Yi-Chia Wu, MD2, Andrew Korman, MD2. B0421 - Case Report: Mycobacterium paragordonae Associated Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
