Back

Poster Session D - Tuesday Morning
Category: Stomach
D0705 - Treating Helicobacter pylori via IV Route in a Patient With Malabsorption Due to Gastric Bypass Surgery
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Mary Alexandra Bramlage, MD
Carolinas Medical Center Atrium Health
Charlotte, NC
Presenting Author(s)
Mary Alexandra Bramlage, MD1, Jessica L. Sang, MD, MPH2, Baharak Moshiree, MD, MSCI, FACG2
1Carolinas Medical Center Atrium Health, Charlotte, NC; 2Atrium Health, Charlotte, NC
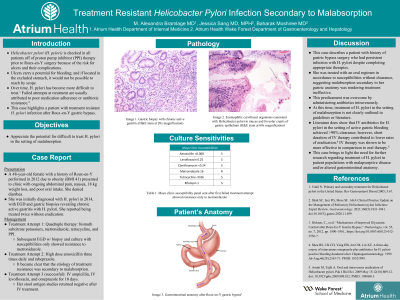
Introduction: Helicobacter pylori (H. pylori) is checked in all patients off of proton pump inhibitor (PPI) therapy prior to Roux-en-Y surgery because of the risk for ulcers and their complications. Ulcers carry a potential for bleeding; and if located in the excluded stomach, it would not be possible to reach by scope. Over time, H. pylori has become more difficult to treat. Failed attempts at treatment are usually attributed to poor medication adherence or antibiotic resistance.1 This case highlights a patient with treatment resistant H. pylori infection after Roux-en-Y gastric bypass.
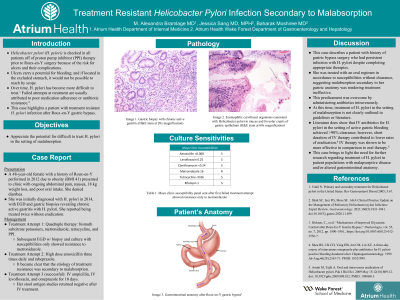
Case Description/Methods: A 48-year-old female with a history of Roux-en-Y performed in 2012 due to obesity presented to clinic with ongoing abdominal pain, nausea, 18 kg weight loss, and poor oral intake. She was initially diagnosed with H. pylori in 2014, with EGD and gastric biopsies revealing chronic active gastritis with H. pylori. She reported being treated twice without eradication. Repeat EGD took place in 2020 with persistent H. pylori on biopsy. She was prescribed quadruple therapy: bismuth subcitrate potassium, metronidazole, tetracycline, and PPI. Despite this, she did not clear the infection. She was re-biopsied and tissue specimen was sent for susceptibility. Results only showed resistance to metronidazole. Based on susceptibilities, she was prescribed high dose amoxicillin three times daily and rabeprazole. Despite appropriate therapy, she tested positive once again. It became clear that the etiology of treatment resistance was secondary to malabsorption. She was ultimately treated with IV ampicillin, IV levofloxacin, and omeprazole for 10 days. Finally, her stool antigen studies returned negative.
Discussion: This case describes a patient with history of gastric bypass surgery who had persistent infection with H. pylori despite completing appropriate therapies. She was treated with an oral regimen in accordance to susceptibilities without clearance, suggesting malabsorption secondary to her gastric anatomy was rendering treatment ineffective. This predicament was overcome by administering antibiotics intravenously. This case brings to light the need for further research regarding treatment of H. pylori in the setting of malabsorption, as this not clearly outlined in current guidelines or literature.
1. Shah SC, Iyer PG, Moss SF. AGA Clinical Practice Update on the Management of Refractory H pylori Infection: Expert Review. Gastroenterology. 2021;160(5):1831-1841. doi:10.1053/j.gastro.2020.11.059
Disclosures:
Mary Alexandra Bramlage, MD1, Jessica L. Sang, MD, MPH2, Baharak Moshiree, MD, MSCI, FACG2. D0705 - Treating Helicobacter pylori via IV Route in a Patient With Malabsorption Due to Gastric Bypass Surgery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Carolinas Medical Center Atrium Health, Charlotte, NC; 2Atrium Health, Charlotte, NC
Introduction: Helicobacter pylori (H. pylori) is checked in all patients off of proton pump inhibitor (PPI) therapy prior to Roux-en-Y surgery because of the risk for ulcers and their complications. Ulcers carry a potential for bleeding; and if located in the excluded stomach, it would not be possible to reach by scope. Over time, H. pylori has become more difficult to treat. Failed attempts at treatment are usually attributed to poor medication adherence or antibiotic resistance.1 This case highlights a patient with treatment resistant H. pylori infection after Roux-en-Y gastric bypass.
Case Description/Methods: A 48-year-old female with a history of Roux-en-Y performed in 2012 due to obesity presented to clinic with ongoing abdominal pain, nausea, 18 kg weight loss, and poor oral intake. She was initially diagnosed with H. pylori in 2014, with EGD and gastric biopsies revealing chronic active gastritis with H. pylori. She reported being treated twice without eradication. Repeat EGD took place in 2020 with persistent H. pylori on biopsy. She was prescribed quadruple therapy: bismuth subcitrate potassium, metronidazole, tetracycline, and PPI. Despite this, she did not clear the infection. She was re-biopsied and tissue specimen was sent for susceptibility. Results only showed resistance to metronidazole. Based on susceptibilities, she was prescribed high dose amoxicillin three times daily and rabeprazole. Despite appropriate therapy, she tested positive once again. It became clear that the etiology of treatment resistance was secondary to malabsorption. She was ultimately treated with IV ampicillin, IV levofloxacin, and omeprazole for 10 days. Finally, her stool antigen studies returned negative.
Discussion: This case describes a patient with history of gastric bypass surgery who had persistent infection with H. pylori despite completing appropriate therapies. She was treated with an oral regimen in accordance to susceptibilities without clearance, suggesting malabsorption secondary to her gastric anatomy was rendering treatment ineffective. This predicament was overcome by administering antibiotics intravenously. This case brings to light the need for further research regarding treatment of H. pylori in the setting of malabsorption, as this not clearly outlined in current guidelines or literature.
1. Shah SC, Iyer PG, Moss SF. AGA Clinical Practice Update on the Management of Refractory H pylori Infection: Expert Review. Gastroenterology. 2021;160(5):1831-1841. doi:10.1053/j.gastro.2020.11.059
Disclosures:
Mary Alexandra Bramlage indicated no relevant financial relationships.
Jessica Sang indicated no relevant financial relationships.
Baharak Moshiree indicated no relevant financial relationships.
Mary Alexandra Bramlage, MD1, Jessica L. Sang, MD, MPH2, Baharak Moshiree, MD, MSCI, FACG2. D0705 - Treating Helicobacter pylori via IV Route in a Patient With Malabsorption Due to Gastric Bypass Surgery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
