Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0047 - A Double Take on a 20-Year Double J-Stent
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Daniel Stenberg, DO
University of Washington
Mill Creek, WA
Presenting Author(s)
Daniel Stenberg, DO1, Galvin Dhaliwal, MD2, Mohammed Alkhero, MD3, Mladen Jecmenica, MD4
1University of Washington, Temecula, CA; 2UHS SoCal MEC, Temecula, CA; 3Temecula Valley Hospital, Temecula, CA; 4Corona Regional Medical Center, Corona, CA
Introduction: The double J biliary stent is commonly used to relieve obstructions and aid in draining of pancreatic fluid. Indwelling or forgotten stents are rarely seen and their sequelae are unknown. We present the case of a patient who was lost to follow-up over twenty years ago following cholecystectomy and placement of double J stent. A routine esophagogastroduodenoscopy (EGD) for variceal surveillance was performed and discovered an ampullary fungating mass.
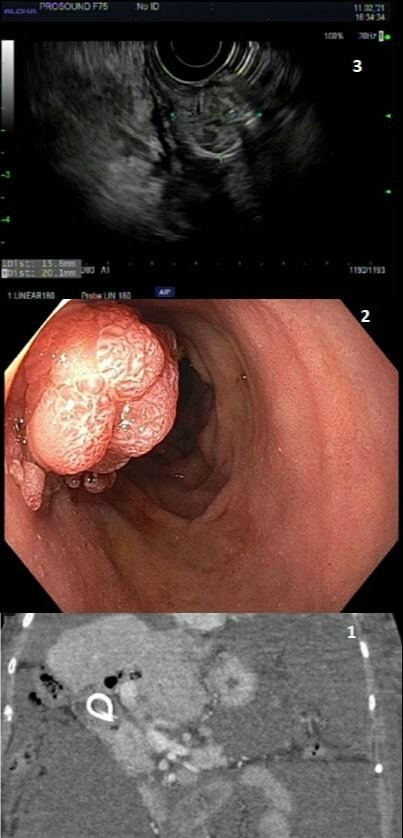
Case Description/Methods: A 79 y/o female with a history of hypertension presented to the ED with worsening abdominal distention. She was a poor historian but denied alcohol use, drug use, or any history of liver disease. Her workup included an abdominal paracentesis removing greater than 7 liters of fluid with a SAAG indicating portal hypertension. She had abnormal liver function tests (LFTs) and CT imaging was consistent with cirrhotic morphology of the liver and a double-J stent present in CBD [Figure 1]. An EGD for further evaluation and for variceal vein monitoring was done revealing grade 2 varices but more significantly, at the site of ampulla of vater a large fungating mass was noted. The mass was medium-sized and polypoid with no bleeding. The CBD stent was in place with noted hyperproliferation of the tissue of the ampulla vs a periampullar duodenal mass [Figure 2]. A repeat EDG with EUS was performed, finding the hypoechoic non-circumferential mass endosonographically within the ampulla. The mass measured 24 mm by 14 mm in maximal cross-sectional diameter [Figure 3]. The lesion extended from the mucosa to the muscularis mucosa. The endosonographic borders were well-defined. There was sonographic evidence suggesting invasion into the deep mucosa (Layer 2). Filamentous microorganisms were identified on HE and GMS stain. No individual atypical AE1/AE3 positive epithelial cells were identified.
Discussion: This case highlights the unusual sequelae of a retained double-J stent in a patient who was lost to follow up. It’s unknown why the stent was placed, likely during an intraoperative cholangiogram, and the patient did not recall her follow-up instructions. Several questions arise surrounding the mass such as, did it have malignant potential and what role, if any, did the stent have in the formation of the mass? Did colonization represent an increased risk of ascending cholangitis? The stent was left in at the conclusion of the case and the patient was extensively educated about follow-up and maintenance endoscopy
Disclosures:
Daniel Stenberg, DO1, Galvin Dhaliwal, MD2, Mohammed Alkhero, MD3, Mladen Jecmenica, MD4. C0047 - A Double Take on a 20-Year Double J-Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Washington, Temecula, CA; 2UHS SoCal MEC, Temecula, CA; 3Temecula Valley Hospital, Temecula, CA; 4Corona Regional Medical Center, Corona, CA
Introduction: The double J biliary stent is commonly used to relieve obstructions and aid in draining of pancreatic fluid. Indwelling or forgotten stents are rarely seen and their sequelae are unknown. We present the case of a patient who was lost to follow-up over twenty years ago following cholecystectomy and placement of double J stent. A routine esophagogastroduodenoscopy (EGD) for variceal surveillance was performed and discovered an ampullary fungating mass.
Case Description/Methods: A 79 y/o female with a history of hypertension presented to the ED with worsening abdominal distention. She was a poor historian but denied alcohol use, drug use, or any history of liver disease. Her workup included an abdominal paracentesis removing greater than 7 liters of fluid with a SAAG indicating portal hypertension. She had abnormal liver function tests (LFTs) and CT imaging was consistent with cirrhotic morphology of the liver and a double-J stent present in CBD [Figure 1]. An EGD for further evaluation and for variceal vein monitoring was done revealing grade 2 varices but more significantly, at the site of ampulla of vater a large fungating mass was noted. The mass was medium-sized and polypoid with no bleeding. The CBD stent was in place with noted hyperproliferation of the tissue of the ampulla vs a periampullar duodenal mass [Figure 2]. A repeat EDG with EUS was performed, finding the hypoechoic non-circumferential mass endosonographically within the ampulla. The mass measured 24 mm by 14 mm in maximal cross-sectional diameter [Figure 3]. The lesion extended from the mucosa to the muscularis mucosa. The endosonographic borders were well-defined. There was sonographic evidence suggesting invasion into the deep mucosa (Layer 2). Filamentous microorganisms were identified on HE and GMS stain. No individual atypical AE1/AE3 positive epithelial cells were identified.
Discussion: This case highlights the unusual sequelae of a retained double-J stent in a patient who was lost to follow up. It’s unknown why the stent was placed, likely during an intraoperative cholangiogram, and the patient did not recall her follow-up instructions. Several questions arise surrounding the mass such as, did it have malignant potential and what role, if any, did the stent have in the formation of the mass? Did colonization represent an increased risk of ascending cholangitis? The stent was left in at the conclusion of the case and the patient was extensively educated about follow-up and maintenance endoscopy
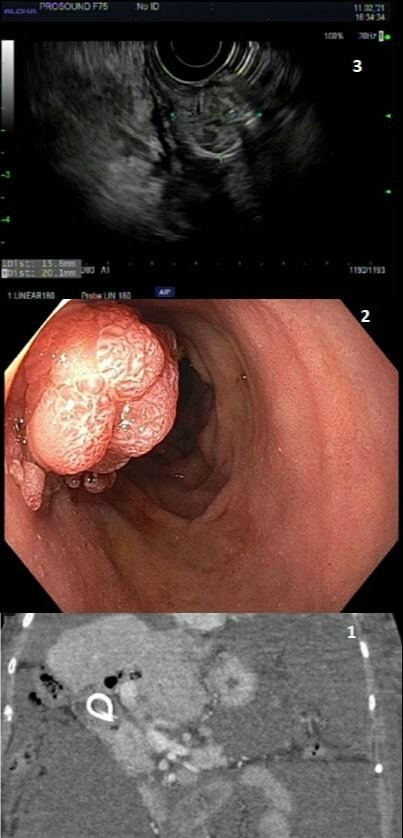
Figure: Figures 1, 2, and 3 demonstrating CT evidence of pneumobilia, ampullary fungating mass, and EUS imaging
Disclosures:
Daniel Stenberg indicated no relevant financial relationships.
Galvin Dhaliwal indicated no relevant financial relationships.
Mohammed Alkhero indicated no relevant financial relationships.
Mladen Jecmenica indicated no relevant financial relationships.
Daniel Stenberg, DO1, Galvin Dhaliwal, MD2, Mohammed Alkhero, MD3, Mladen Jecmenica, MD4. C0047 - A Double Take on a 20-Year Double J-Stent, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
