Back

Poster Session A - Sunday Afternoon
Category: Colon
A0151 - Systemic Mastocytosis Presented as Subtle Colonic Mucosa Change
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Haoran Peng, MD
Augusta University Medical College of Georgia
Augusta, GA
Presenting Author(s)
Haroon Alam, MD1, Haoran Peng, MD2, Matthew R. Powell, MD3, Taylor Sliker, MD2, Humberto Sifuentes, MD2
1Morehouse School of Medicine, Atlanta, GA; 2Augusta University Medical College of Georgia, Augusta, GA; 3Medical College of Georgia, Augusta, GA
Introduction: Mastocytosis is a rare disease that result from clonal proliferation of abnormal mast cells in various organ systems including skin, liver, lymph nodes, spleen, bone marrow, and mucosal surfaces. Gastrointestinal (GI) involvement occurs in about 14-85% of the cases. Here, we report a case of indolent systemic mastocytosis presented as subtle colonic mucosa nodularity.
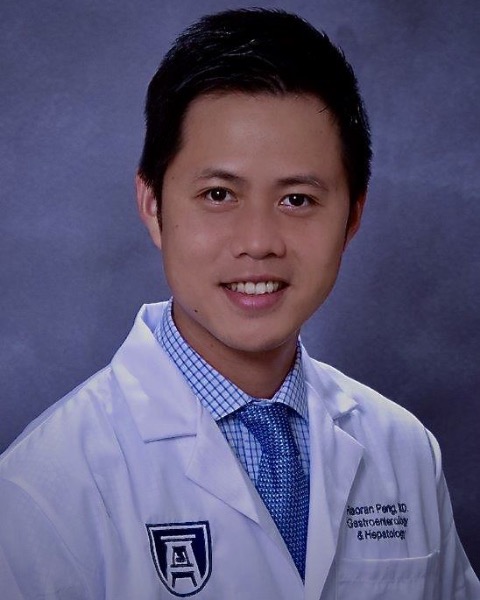
Case Description/Methods: A 69-year-old Caucasian lady with PMH of Stage IIB ovary low grade serous carcinoma s/p chemotherapy in remission presented for surveillance colonoscopy due to history of colon polyps. Cecum revealed nodularity change found in cecum and sigmoid colon. Biopsies were performed and showed atypical mast cell proliferation. The patient was reassessed but denied allergy history, or any GI symptoms. Previous colonoscopy did not show mast cell disease. She was referred to hematology for bone marrow biopsy. Labs including CBC with differential were normal but tryptase level was 26.7 (normal range < 11.5). Bone marrow biopsy and cytogenetic analysis revealed no clonal chromosome abnormalities, normal karyotype, hypercellular marrow with maturing trilineage hematopoiesis, and polytopic B-cells. Histopathology showed increased response to C-kit and CD25, concerning for systemic mastocytosis. Patient lacks systemic involvement, and her disease would be considered indolent, thereby only requiring surveillance at this time.
Discussion: Mastocytosis is a rare disease that affects approximately 1 in 10,000 people in the United States. It is defined as an abnormal increase in mast cells and can present in many ways. Cutaneous mastocytosis is limited to the skin while systemic mastocytosis infiltrates the bone marrow and other organ systems including GI tract. Common GI symptoms include nausea, vomit, abdominal pain, diarrhea. Diagnosis of mastocytosis is based on Word Health Organization criteria (table 1). It requires bone marrow biopsy and biopsies of affected organs with dense infiltrates of mast cells. Elevated serum tryptase >20, KIT mutation, presence of CD2 and/or CD25 would support the diagnosis. Treatment depends on the severity of the disease. Severe systemic mastocytosis or mast cell leukemia may require chemotherapy or stem cell transplant. But indolent mastocytosis, as in our case, requires routine surveillance with CBC with differential, liver enzymes, immunoglobulin levels, and DEXA scan. Our case highlights the importance of sampling subtle abnormal GI mucosal findings during the procedures.
Disclosures:
Haroon Alam, MD1, Haoran Peng, MD2, Matthew R. Powell, MD3, Taylor Sliker, MD2, Humberto Sifuentes, MD2. A0151 - Systemic Mastocytosis Presented as Subtle Colonic Mucosa Change, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Morehouse School of Medicine, Atlanta, GA; 2Augusta University Medical College of Georgia, Augusta, GA; 3Medical College of Georgia, Augusta, GA
Introduction: Mastocytosis is a rare disease that result from clonal proliferation of abnormal mast cells in various organ systems including skin, liver, lymph nodes, spleen, bone marrow, and mucosal surfaces. Gastrointestinal (GI) involvement occurs in about 14-85% of the cases. Here, we report a case of indolent systemic mastocytosis presented as subtle colonic mucosa nodularity.
Case Description/Methods: A 69-year-old Caucasian lady with PMH of Stage IIB ovary low grade serous carcinoma s/p chemotherapy in remission presented for surveillance colonoscopy due to history of colon polyps. Cecum revealed nodularity change found in cecum and sigmoid colon. Biopsies were performed and showed atypical mast cell proliferation. The patient was reassessed but denied allergy history, or any GI symptoms. Previous colonoscopy did not show mast cell disease. She was referred to hematology for bone marrow biopsy. Labs including CBC with differential were normal but tryptase level was 26.7 (normal range < 11.5). Bone marrow biopsy and cytogenetic analysis revealed no clonal chromosome abnormalities, normal karyotype, hypercellular marrow with maturing trilineage hematopoiesis, and polytopic B-cells. Histopathology showed increased response to C-kit and CD25, concerning for systemic mastocytosis. Patient lacks systemic involvement, and her disease would be considered indolent, thereby only requiring surveillance at this time.
Discussion: Mastocytosis is a rare disease that affects approximately 1 in 10,000 people in the United States. It is defined as an abnormal increase in mast cells and can present in many ways. Cutaneous mastocytosis is limited to the skin while systemic mastocytosis infiltrates the bone marrow and other organ systems including GI tract. Common GI symptoms include nausea, vomit, abdominal pain, diarrhea. Diagnosis of mastocytosis is based on Word Health Organization criteria (table 1). It requires bone marrow biopsy and biopsies of affected organs with dense infiltrates of mast cells. Elevated serum tryptase >20, KIT mutation, presence of CD2 and/or CD25 would support the diagnosis. Treatment depends on the severity of the disease. Severe systemic mastocytosis or mast cell leukemia may require chemotherapy or stem cell transplant. But indolent mastocytosis, as in our case, requires routine surveillance with CBC with differential, liver enzymes, immunoglobulin levels, and DEXA scan. Our case highlights the importance of sampling subtle abnormal GI mucosal findings during the procedures.
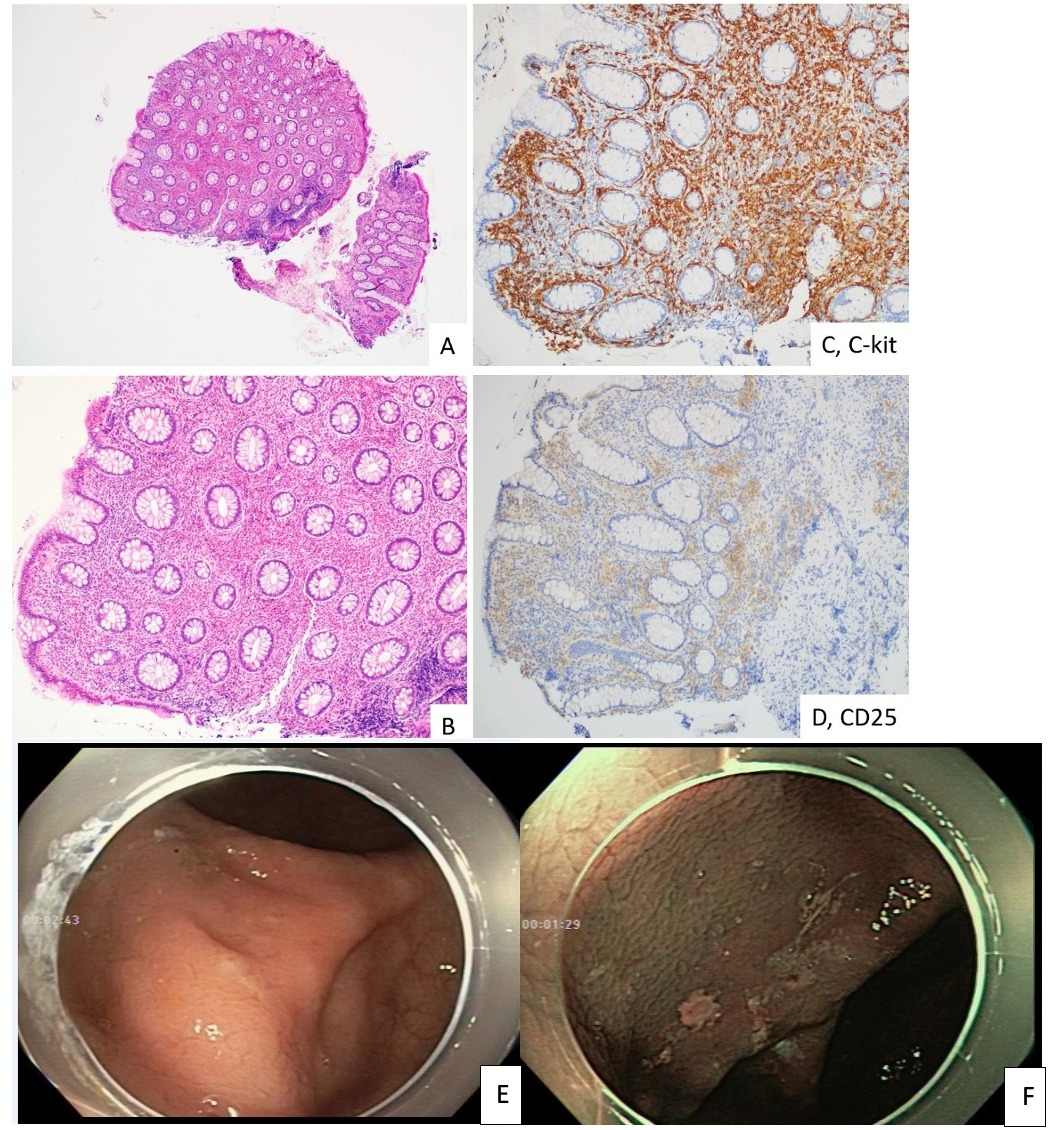
Figure: (Figures A-B): Biopsy of both polyps showed polypoid colonic mucosa with a lamina propria expanded by atypical clusters of spindled mast cells and prominent background eosinophilia. (Figure C): Immunohistochemistry for C-kit/CD117 confirmed a marked increase in clustered and spindled mast cells. (Figure D): CD25 was also positive in the mast cells, a marker typically positive in systemic mastocytosis. (Figure E): Cecal picture with very subtle nodularity change. (Figure F): NBI picture of nodularity change in cecum.
Disclosures:
Haroon Alam indicated no relevant financial relationships.
Haoran Peng indicated no relevant financial relationships.
Matthew Powell indicated no relevant financial relationships.
Taylor Sliker indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Haroon Alam, MD1, Haoran Peng, MD2, Matthew R. Powell, MD3, Taylor Sliker, MD2, Humberto Sifuentes, MD2. A0151 - Systemic Mastocytosis Presented as Subtle Colonic Mucosa Change, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
