Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0483 - Disparities in the Prevalence of Acute Myocardial Infarction in Non-Alcoholic Steatohepatitis: A Nationwide Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Umar Hayat, MBBS
University of Kansas
Duryea, PA
Presenting Author(s)
Umar Hayat, MBBS1, Maham Waqar, MBBS2, Fnu Faheela, MBBS3, Muhammad Kamal, MD4, Cyrus Munguti, MD1, Hayrettin Okut, PhD1, Tariq Ahmad, MD5, Muhammad Haseeb, MD, MSc6
1University of Kansas, Wichita, KS; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Essen Healthcare System, New York, NY; 5Geisinger Wyoming Valley Hospital Northeast, Wilkes-Barre, PA; 6Beth Israel Deaconess Medical Center, Boston, MA
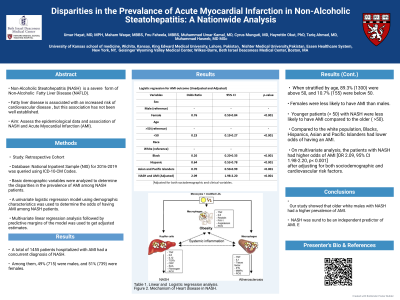
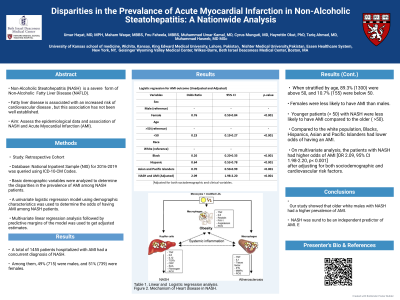
Introduction: Non-Alcoholic Steatohepatitis (NASH) is a severe form of Non-Alcoholic Fatty Liver Disease (NAFLD) characterized by intrahepatic and extrahepatic inflammation. Fatty liver disease is also associated with an increased risk of cardiovascular disease, but this association has not been well established. Our study aimed to assess the epidemiological data and association of NASH with Acute Myocardial Infarction (AMI).
Methods: The National Inpatient Sample (NIS) database 2016-2019 was queried using (ICD10-CM) codes to identify a cohort of inpatient admissions with a primary diagnosis of AMI and secondary diagnosis of NASH. Basic demographic variables were analyzed to determine the disparities in the prevalence of AMI among NASH patients. A univariate logistic regression model using demographic characteristics was used to determine the odds of having AMI among NASH patients. Multivariate logistic regression analysis was used to analyze the association of NASH and AMI.
Results: A total of 1455 patients hospitalized with AMI had a concurrent diagnosis of NASH. Among them, 49% (715) were males, and 51% (739) were females. Females were less likely to have AMI than males [OR 0.76, 95% CI 0.59-0.84]. When stratified by age, 89.3% (1300) were above 50, and 10.7% (155) were below 50. Younger patients (< 50) with NASH were less likely to have AMI compared to the older ( >50) [OR 0.23, 95% CI 0.19-0.27, p< 0.001]. When stratified for the race, 78.83% (1147) were white, 4.6% (67) were Black, 8.4% (122) were Hispanic, 2.26% (33) were Asian or Pacific Islander, 0.89% (13) were Native Americans. Compared to the white population, Blacks [OR 0.26, 95% CI 0.20-0.33, p< 0.001], Hispanics [OR 0.64, 95% CI 0.53-0.78, p< 0.001], Asian and Pacific Islanders [OR 0.70, 95% CI 0.50-0.99, p< 0.001], had lower odds of having an AMI. On multivariate analysis, the patients with NASH had higher odds of AMI [OR 2.09, 95% CI 1.98-2.20, p< 0.001] after adjusting for both sociodemographic and cardiovascular risk factors.
Discussion: Our study showed that older white males with NASH had a higher prevalence of AMI. In addition, NASH was found to be an independent predictor of AMI. Early identification of risk factors and an aggressive cardiovascular risk modification are required among NASH patients. Future prospective studies with better cohort stratification are required to validate this association.
Disclosures:
Umar Hayat, MBBS1, Maham Waqar, MBBS2, Fnu Faheela, MBBS3, Muhammad Kamal, MD4, Cyrus Munguti, MD1, Hayrettin Okut, PhD1, Tariq Ahmad, MD5, Muhammad Haseeb, MD, MSc6. E0483 - Disparities in the Prevalence of Acute Myocardial Infarction in Non-Alcoholic Steatohepatitis: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kansas, Wichita, KS; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Essen Healthcare System, New York, NY; 5Geisinger Wyoming Valley Hospital Northeast, Wilkes-Barre, PA; 6Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Non-Alcoholic Steatohepatitis (NASH) is a severe form of Non-Alcoholic Fatty Liver Disease (NAFLD) characterized by intrahepatic and extrahepatic inflammation. Fatty liver disease is also associated with an increased risk of cardiovascular disease, but this association has not been well established. Our study aimed to assess the epidemiological data and association of NASH with Acute Myocardial Infarction (AMI).
Methods: The National Inpatient Sample (NIS) database 2016-2019 was queried using (ICD10-CM) codes to identify a cohort of inpatient admissions with a primary diagnosis of AMI and secondary diagnosis of NASH. Basic demographic variables were analyzed to determine the disparities in the prevalence of AMI among NASH patients. A univariate logistic regression model using demographic characteristics was used to determine the odds of having AMI among NASH patients. Multivariate logistic regression analysis was used to analyze the association of NASH and AMI.
Results: A total of 1455 patients hospitalized with AMI had a concurrent diagnosis of NASH. Among them, 49% (715) were males, and 51% (739) were females. Females were less likely to have AMI than males [OR 0.76, 95% CI 0.59-0.84]. When stratified by age, 89.3% (1300) were above 50, and 10.7% (155) were below 50. Younger patients (< 50) with NASH were less likely to have AMI compared to the older ( >50) [OR 0.23, 95% CI 0.19-0.27, p< 0.001]. When stratified for the race, 78.83% (1147) were white, 4.6% (67) were Black, 8.4% (122) were Hispanic, 2.26% (33) were Asian or Pacific Islander, 0.89% (13) were Native Americans. Compared to the white population, Blacks [OR 0.26, 95% CI 0.20-0.33, p< 0.001], Hispanics [OR 0.64, 95% CI 0.53-0.78, p< 0.001], Asian and Pacific Islanders [OR 0.70, 95% CI 0.50-0.99, p< 0.001], had lower odds of having an AMI. On multivariate analysis, the patients with NASH had higher odds of AMI [OR 2.09, 95% CI 1.98-2.20, p< 0.001] after adjusting for both sociodemographic and cardiovascular risk factors.
Discussion: Our study showed that older white males with NASH had a higher prevalence of AMI. In addition, NASH was found to be an independent predictor of AMI. Early identification of risk factors and an aggressive cardiovascular risk modification are required among NASH patients. Future prospective studies with better cohort stratification are required to validate this association.
Disclosures:
Umar Hayat indicated no relevant financial relationships.
Maham Waqar indicated no relevant financial relationships.
Fnu Faheela indicated no relevant financial relationships.
Muhammad Kamal indicated no relevant financial relationships.
Cyrus Munguti indicated no relevant financial relationships.
Hayrettin Okut indicated no relevant financial relationships.
Tariq Ahmad indicated no relevant financial relationships.
Muhammad Haseeb indicated no relevant financial relationships.
Umar Hayat, MBBS1, Maham Waqar, MBBS2, Fnu Faheela, MBBS3, Muhammad Kamal, MD4, Cyrus Munguti, MD1, Hayrettin Okut, PhD1, Tariq Ahmad, MD5, Muhammad Haseeb, MD, MSc6. E0483 - Disparities in the Prevalence of Acute Myocardial Infarction in Non-Alcoholic Steatohepatitis: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
