Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0241 - A Case Report of Volatile Ingestion-Induced Acute Esophageal Necrosis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Elizabeth A. Rowland, MD, MBA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Elizabeth A. Rowland, MD, MBA, Kelly Zucker, DO, Yasmin Alishahi, MD, FACG
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Acute esophageal necrosis (AEN), also known as black esophagus or acute necrotizing esophagitis, is a rare syndrome with diffuse circumferential black discoloration often of distal third esophageal mucosa due to relative hypovascularity and termination at the gastro-esophageal junction. It usually presents with upper GI hemorrhage. Despite controversial pathogenesis, there is strong consideration for a two-hit hypothesis where an initial low-flow vascular state predisposes the mucosa to a severe topical injury. Chemical injury by gastric contents, toxin ingestion, severe infectious diseases, diabetic ketoacidosis and shock are associated with AEN. Advanced age, male gender and comorbidities like diabetes mellitus (DM), hypertension, cardiovascular disease, chronic kidney disease, malnutrition, chronic alcohol abuse, post-irradiation are predisposing risk factors for AEN. We present a patient with a favorable outcome of a generally rare, life-threatening condition due to early recognition and treatment.
Case Description/Methods: A 74-year-old male presented to the hospital with shock and 3-day history of hematemesis. He had history of coronary artery disease, Type II Diabetes Mellitus, chronic obstructive pulmonary disease, esophageal adenocarcinoma post chemotherapy and radiation complicated by erosive esophagitis and alcoholism.
Labs were significant for acute kidney injury (AKI), high anion gap metabolic acidosis (HAGMA), osmolar gap of 59 mOsm/kg and hemoglobin drop from 14 to 9 g/dL. Volatile panel not sent; drug-screen benign, infectious work-up negative. CT abdomen had distended stomach; thus, NG tube placed for decompression, yielding 700cc of coffee ground emesis. Upper endoscopy performed 2-days later showed Los Angeles Grade D esophagitis with entire esophagus with black appearance, gastric body erosions and superficial clean-based duodenal ulcers. Patient was continued on PPI twice daily for 8 weeks with planned repeat EGD.
Discussion: This patient likely had volatile ingestion chemical injury given shock, hematemesis, AKI with HAGMA and osmolar gap. Despite AEN’s rarity with prevalence of 0.2 percent in autopsy states, given overall 32 percent mortality rate and 6 percent mortality rate directly attributed to complications of AEN, early recognition and prompt medical management is imperative for favorable outcomes. Treatment focuses on supportive therapy: namely resuscitation, PPIs, sucralfate, keeping the patient NPO and avoiding nasogastric tube to avoid esophageal perforation.
Disclosures:
Elizabeth A. Rowland, MD, MBA, Kelly Zucker, DO, Yasmin Alishahi, MD, FACG. C0241 - A Case Report of Volatile Ingestion-Induced Acute Esophageal Necrosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Acute esophageal necrosis (AEN), also known as black esophagus or acute necrotizing esophagitis, is a rare syndrome with diffuse circumferential black discoloration often of distal third esophageal mucosa due to relative hypovascularity and termination at the gastro-esophageal junction. It usually presents with upper GI hemorrhage. Despite controversial pathogenesis, there is strong consideration for a two-hit hypothesis where an initial low-flow vascular state predisposes the mucosa to a severe topical injury. Chemical injury by gastric contents, toxin ingestion, severe infectious diseases, diabetic ketoacidosis and shock are associated with AEN. Advanced age, male gender and comorbidities like diabetes mellitus (DM), hypertension, cardiovascular disease, chronic kidney disease, malnutrition, chronic alcohol abuse, post-irradiation are predisposing risk factors for AEN. We present a patient with a favorable outcome of a generally rare, life-threatening condition due to early recognition and treatment.
Case Description/Methods: A 74-year-old male presented to the hospital with shock and 3-day history of hematemesis. He had history of coronary artery disease, Type II Diabetes Mellitus, chronic obstructive pulmonary disease, esophageal adenocarcinoma post chemotherapy and radiation complicated by erosive esophagitis and alcoholism.
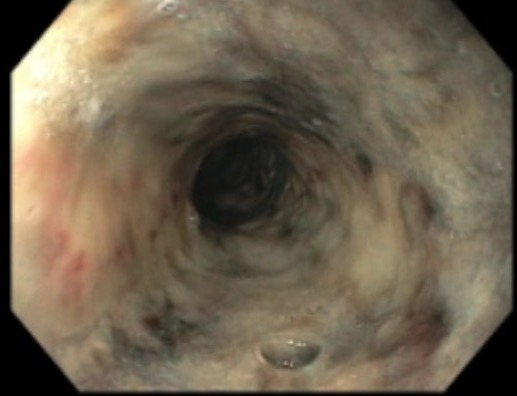
Labs were significant for acute kidney injury (AKI), high anion gap metabolic acidosis (HAGMA), osmolar gap of 59 mOsm/kg and hemoglobin drop from 14 to 9 g/dL. Volatile panel not sent; drug-screen benign, infectious work-up negative. CT abdomen had distended stomach; thus, NG tube placed for decompression, yielding 700cc of coffee ground emesis. Upper endoscopy performed 2-days later showed Los Angeles Grade D esophagitis with entire esophagus with black appearance, gastric body erosions and superficial clean-based duodenal ulcers. Patient was continued on PPI twice daily for 8 weeks with planned repeat EGD.
Discussion: This patient likely had volatile ingestion chemical injury given shock, hematemesis, AKI with HAGMA and osmolar gap. Despite AEN’s rarity with prevalence of 0.2 percent in autopsy states, given overall 32 percent mortality rate and 6 percent mortality rate directly attributed to complications of AEN, early recognition and prompt medical management is imperative for favorable outcomes. Treatment focuses on supportive therapy: namely resuscitation, PPIs, sucralfate, keeping the patient NPO and avoiding nasogastric tube to avoid esophageal perforation.
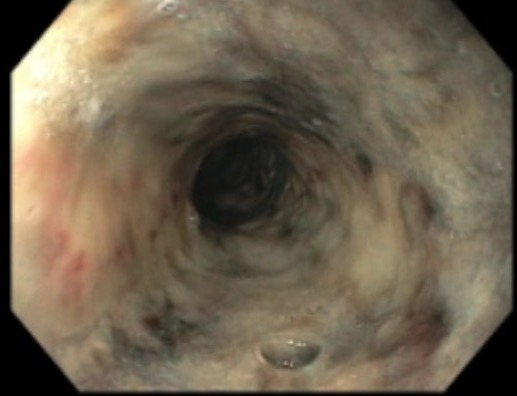
Figure: Proximal Acute Esophageal Necrosis
Disclosures:
Elizabeth Rowland indicated no relevant financial relationships.
Kelly Zucker indicated no relevant financial relationships.
Yasmin Alishahi indicated no relevant financial relationships.
Elizabeth A. Rowland, MD, MBA, Kelly Zucker, DO, Yasmin Alishahi, MD, FACG. C0241 - A Case Report of Volatile Ingestion-Induced Acute Esophageal Necrosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
