Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0061 - A Case of Silent Cancer: CT Negative Ampullary Adenocarcinoma
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- KA
Kamal Amer, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Kamal Amer, MD1, Alaa Musallam, MD2, Thomas Pustorino, MD3, Brooke Baker, MS, MD4, Sushil Ahlawat, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers, Clifton, NJ; 3Atlantic Healthcare, Summit, NJ; 4Rutgers-New Jersey Medical School, Newark, NJ
Introduction: Ampullary cancers are rare and account for approximately 0.2% of gastrointestinal cancers. These patients tend to have an improved prognosis as they typically present early and can often be diagnosed with imaging, leading to higher surgical resection rates than other pancreatobiliary malignancies. Early detection is crucial as surgical resection can be curative.
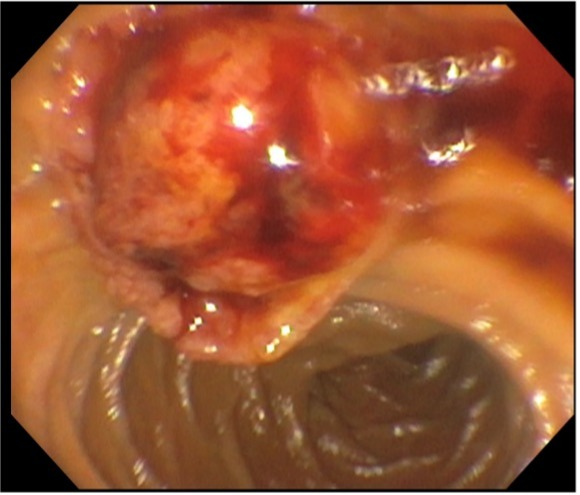
Case Description/Methods: A 59-year-old male with a history of hypertension and a prior cerebrovascular accident presented with 6 weeks of painless jaundice. He experienced itching, diarrhea, bloating, fatigue and 4–5-pound weight loss for the same duration of time. Initial labs showed a total bilirubin of 19.9, direct bilirubin of 14.7, alkaline phosphatase of 203, ALT of 112 and AST of 112. CT with IV contrast showed intra and extra-hepatic dilatation with the common bile duct greater than 20 mm. There was no evidence of biliary mass or pancreatic mass noted. The patient underwent ERCP where a large (5cm x 3cm) fungating ulcerated lesion was found (Figure 1). The mass was friable and appeared to extend into the biliary duct. Three 8 French by 9.5 cm plastic stents were placed into the common bile duct. Biopsies were obtained and the pathology resulted as adenocarcinoma.
Discussion: Ampullary adenocarcinoma is rare, with an incidence of 0.70 per 100,000 men and 0.45 per 100,000 women in the US. These patients present with symptoms of biliary obstruction and radiographic imaging demonstrating the double duct sign. Often imaging also demonstrates a discrete nodular mass that produces a filling defect at the pancreaticobiliary junction. In some cases, despite the presence of ductal dilation, there is no evidence of an obstructing mass, even on endoscopic evaluation, and a diagnosis is made solely through biopsy.
Our patient presented with symptoms of obstructive jaundice with CT evidence of biliary and pancreatic duct dilation without radiographic evidence of a mass. Only through ERCP were we able to identify the large mass, which was diagnosed as adenocarcinoma. This case did not follow the typical presentation, as a mass was not seen on imaging and could have delayed diagnosis and treatment. We recommend the addition of diffusion weighted imaging to the diagnostic algorithm as it has been shown to improve the detection rate when compared to conventional imaging.
Disclosures:
Kamal Amer, MD1, Alaa Musallam, MD2, Thomas Pustorino, MD3, Brooke Baker, MS, MD4, Sushil Ahlawat, MD1. D0061 - A Case of Silent Cancer: CT Negative Ampullary Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Rutgers, Clifton, NJ; 3Atlantic Healthcare, Summit, NJ; 4Rutgers-New Jersey Medical School, Newark, NJ
Introduction: Ampullary cancers are rare and account for approximately 0.2% of gastrointestinal cancers. These patients tend to have an improved prognosis as they typically present early and can often be diagnosed with imaging, leading to higher surgical resection rates than other pancreatobiliary malignancies. Early detection is crucial as surgical resection can be curative.
Case Description/Methods: A 59-year-old male with a history of hypertension and a prior cerebrovascular accident presented with 6 weeks of painless jaundice. He experienced itching, diarrhea, bloating, fatigue and 4–5-pound weight loss for the same duration of time. Initial labs showed a total bilirubin of 19.9, direct bilirubin of 14.7, alkaline phosphatase of 203, ALT of 112 and AST of 112. CT with IV contrast showed intra and extra-hepatic dilatation with the common bile duct greater than 20 mm. There was no evidence of biliary mass or pancreatic mass noted. The patient underwent ERCP where a large (5cm x 3cm) fungating ulcerated lesion was found (Figure 1). The mass was friable and appeared to extend into the biliary duct. Three 8 French by 9.5 cm plastic stents were placed into the common bile duct. Biopsies were obtained and the pathology resulted as adenocarcinoma.
Discussion: Ampullary adenocarcinoma is rare, with an incidence of 0.70 per 100,000 men and 0.45 per 100,000 women in the US. These patients present with symptoms of biliary obstruction and radiographic imaging demonstrating the double duct sign. Often imaging also demonstrates a discrete nodular mass that produces a filling defect at the pancreaticobiliary junction. In some cases, despite the presence of ductal dilation, there is no evidence of an obstructing mass, even on endoscopic evaluation, and a diagnosis is made solely through biopsy.
Our patient presented with symptoms of obstructive jaundice with CT evidence of biliary and pancreatic duct dilation without radiographic evidence of a mass. Only through ERCP were we able to identify the large mass, which was diagnosed as adenocarcinoma. This case did not follow the typical presentation, as a mass was not seen on imaging and could have delayed diagnosis and treatment. We recommend the addition of diffusion weighted imaging to the diagnostic algorithm as it has been shown to improve the detection rate when compared to conventional imaging.
Figure: Endoscopic view of ampullary mass during ERCP
Disclosures:
Kamal Amer indicated no relevant financial relationships.
Alaa Musallam indicated no relevant financial relationships.
Thomas Pustorino indicated no relevant financial relationships.
Brooke Baker indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Kamal Amer, MD1, Alaa Musallam, MD2, Thomas Pustorino, MD3, Brooke Baker, MS, MD4, Sushil Ahlawat, MD1. D0061 - A Case of Silent Cancer: CT Negative Ampullary Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
