Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0245 - Herpes Simplex Esophagitis Masquerading as Reflux Esophagitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Stefan Odabasic, MD
Trinity Health Livonia
Livonia, MI
Presenting Author(s)
Stefan Odabasic, MD1, Tushar Khanna, MD2, Gunjan Shah, MD1
1Trinity Health Livonia, Livonia, MI; 2St. Mary Mercy Hospital, Livonia, MI
Introduction: Herpes simplex esophagitis (HSE), caused by the herpes simplex virus (HSV), is the 3rd most common cause of esophagitis behind GERD and candida infection. It is seen predominantly in hosts with impaired immunity. HSE may result from reactivation of HSV with spread of the virus to the esophageal mucosa by way of the vagus nerve or by direct extension of oral-pharyngeal infection into the esophagus. Most commonly caused by HSV-1 although HSV-2 has occasionally been reported. Patient’s usually present with odynophagia and/or dysphagia. Lesions are typically found in the lower third of the esophagus and are well circumscribed with a volcano-like appearance.
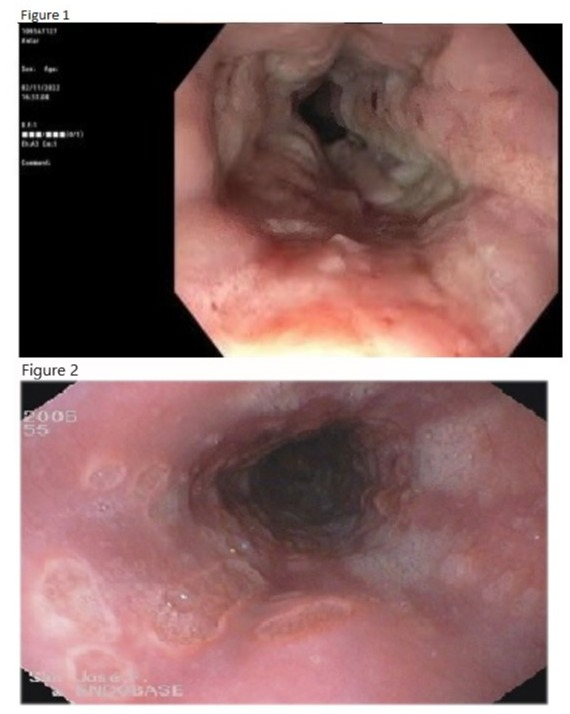
Case Description/Methods: A 78-year-old male with past medical history of CLL, metastatic prostate cancer and MGUS presented with complaints of odynophagia and dysphagia. The patient’s prostate cancer was actively being treated with chemotherapy (Leuprorelin and Docetaxel) so he was empirically started on fluconazole for presumed candida esophagitis. The patient’s labs were not indicative of severe immunosuppression with a normal WBC of 9.3 and ANC of 6.8. He underwent EGD which did not show the characteristic HSE lesions described by Itoh et al. Instead, the patient’s lesions were very typical of reflux esophagitis (Figure 1). However, due to his immunocompromised state, biopsies were sent to check for opportunistic infections. Histology confirmed the diagnosis of HSE and the patient was treated with acyclovir for a total of 21 days. He improved drastically and was able to tolerate diet. He was discharged and scheduled for follow up EGD in 3 months to confirm normalization of the esophagus.
Discussion: Endoscopic findings of HSE have been characterized into type I, II and III by Itoh et al. Types I and II show small punched-out lesions with and without raised margins, respectively (Figure 2). Type III is defined when multiple ulcers became confluent like a map. Vesicular lesions are common in the early stages and exudative lesions are present in most cases. Mucosal necrosis can be seen in the later stages. Our case is interesting because the endoscopic findings were not typical of HSE. The patient was diagnosed with LA grade C reflux esophagitis before pathology confirmed the diagnosis of HSE. This case shows us that opportunistic infections should always be considered in immunocompromised patients even if gross endoscopic appearance does not suggest an infectious cause of esophagitis.
Disclosures:
Stefan Odabasic, MD1, Tushar Khanna, MD2, Gunjan Shah, MD1. E0245 - Herpes Simplex Esophagitis Masquerading as Reflux Esophagitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Trinity Health Livonia, Livonia, MI; 2St. Mary Mercy Hospital, Livonia, MI
Introduction: Herpes simplex esophagitis (HSE), caused by the herpes simplex virus (HSV), is the 3rd most common cause of esophagitis behind GERD and candida infection. It is seen predominantly in hosts with impaired immunity. HSE may result from reactivation of HSV with spread of the virus to the esophageal mucosa by way of the vagus nerve or by direct extension of oral-pharyngeal infection into the esophagus. Most commonly caused by HSV-1 although HSV-2 has occasionally been reported. Patient’s usually present with odynophagia and/or dysphagia. Lesions are typically found in the lower third of the esophagus and are well circumscribed with a volcano-like appearance.
Case Description/Methods: A 78-year-old male with past medical history of CLL, metastatic prostate cancer and MGUS presented with complaints of odynophagia and dysphagia. The patient’s prostate cancer was actively being treated with chemotherapy (Leuprorelin and Docetaxel) so he was empirically started on fluconazole for presumed candida esophagitis. The patient’s labs were not indicative of severe immunosuppression with a normal WBC of 9.3 and ANC of 6.8. He underwent EGD which did not show the characteristic HSE lesions described by Itoh et al. Instead, the patient’s lesions were very typical of reflux esophagitis (Figure 1). However, due to his immunocompromised state, biopsies were sent to check for opportunistic infections. Histology confirmed the diagnosis of HSE and the patient was treated with acyclovir for a total of 21 days. He improved drastically and was able to tolerate diet. He was discharged and scheduled for follow up EGD in 3 months to confirm normalization of the esophagus.
Discussion: Endoscopic findings of HSE have been characterized into type I, II and III by Itoh et al. Types I and II show small punched-out lesions with and without raised margins, respectively (Figure 2). Type III is defined when multiple ulcers became confluent like a map. Vesicular lesions are common in the early stages and exudative lesions are present in most cases. Mucosal necrosis can be seen in the later stages. Our case is interesting because the endoscopic findings were not typical of HSE. The patient was diagnosed with LA grade C reflux esophagitis before pathology confirmed the diagnosis of HSE. This case shows us that opportunistic infections should always be considered in immunocompromised patients even if gross endoscopic appearance does not suggest an infectious cause of esophagitis.
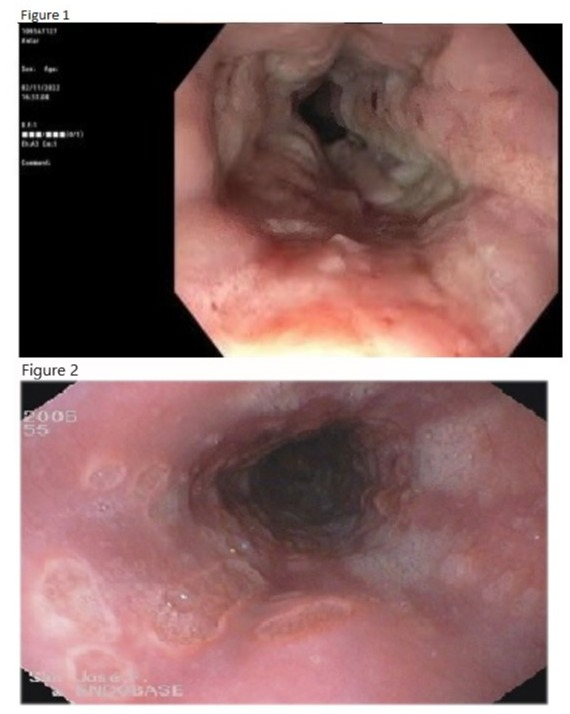
Figure: Figure 1 - EGD images of our patient , diagnosis LA grade C reflux esophagitis
Figure 2 - EGD images of typical herpes simplex esophagitis
Figure 2 - EGD images of typical herpes simplex esophagitis
Disclosures:
Stefan Odabasic indicated no relevant financial relationships.
Tushar Khanna indicated no relevant financial relationships.
Gunjan Shah indicated no relevant financial relationships.
Stefan Odabasic, MD1, Tushar Khanna, MD2, Gunjan Shah, MD1. E0245 - Herpes Simplex Esophagitis Masquerading as Reflux Esophagitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
