Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0494 - Impact of Social Vulnerability Index on Outcomes in Patients With Alcohol-Related Liver Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Ayushi Jain, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Ayushi Jain, MD1, Michael Wellner, MD1, Jing Peng, PhD1, Jianing Ma, PhD1, Kenneth D. Allen, MD1, Chelsey McShane, MD1, Mitchell L. Ramsey, MD1, Sajid Jalil, MBBS1, Khalid Mumtaz, MBBS, MSc2, Sean G. Kelly, MD1, Lanla F. Conteh, MD, MPH, MBA1, Robert Kirkpatrick, MD1, Lindsay A. Sobotka, DO1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Wexner Medical Center, Columbus, OH
Introduction: Alcohol related liver disease affects diverse communities with individual and social characteristics that can impact outcomes. The Social Vulnerability Index (SVI) integrates a range of metrics and assigns a score between 0 and 1, where higher scores represent an increased risk of social vulnerability. Vulnerable patients with alcohol related liver disease have been reported to have worse outcomes. We sought to assess the impact of SVI on outcomes of patients hospitalized with alcohol related liver disease with access to social support services.
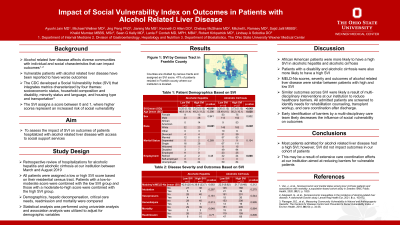
Methods: Hospitalizations for alcohol related liver disease at our institution between March and August 2019 were reviewed. All patients were assigned a low or high SVI score based on their residential census tract. Per our standard practice, patients were screened by multi-disciplinary care coordinators to identify needs for rehabilitation counseling, transplant workup, and care coordination after discharge. Demographics, hepatic decompensation, critical care needs, readmission and mortality were compared.
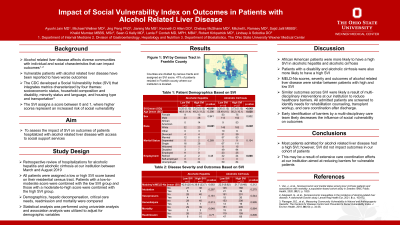
Results: Among 73 patients admitted for alcoholic hepatitis, 32 had a low SVI (mean 0.25) and 42 had a high SVI (mean 0.72). African American patients were more likely to have a higher SVI (35% vs 0%, p=< 0.001). Severity of alcohol hepatitis based on discriminant factor (DF) was similar between high and low SVI patients (mean DF 39.6 vs 42.8, p=0.72). After controlling for race, there was not a significant difference in hepatic decompensation, critical care needs, readmission rate or mortality based on SVI.
There were 393 patients admitted for alcoholic cirrhosis including 166 with a low SVI (mean 0.26) and 227 with a high SVI (mean 0.73). Patients that were African American (23.6% vs 5.5%, p=< 0.001) or disabled (41.4% vs 29.5%, p=0.008) had a higher SVI. MELD-Na scores were similar between the high and low SVI patients (mean MELD-Na 21.7 vs 22.9, p=0.47). After controlling for age, race and employment, there was not a significant difference in hepatic decompensation, critical care needs, readmission rate or mortality based on SVI.
Discussion: Most patients admitted for alcohol related liver disease had a high SVI; however, SVI did not impact outcomes in our cohort of patients. This may be a result of extensive care coordination efforts at our institution aimed at reducing barriers for vulnerable patients. These early interventions likely decrease the effect of SVI on outcomes.
Disclosures:
Ayushi Jain, MD1, Michael Wellner, MD1, Jing Peng, PhD1, Jianing Ma, PhD1, Kenneth D. Allen, MD1, Chelsey McShane, MD1, Mitchell L. Ramsey, MD1, Sajid Jalil, MBBS1, Khalid Mumtaz, MBBS, MSc2, Sean G. Kelly, MD1, Lanla F. Conteh, MD, MPH, MBA1, Robert Kirkpatrick, MD1, Lindsay A. Sobotka, DO1. E0494 - Impact of Social Vulnerability Index on Outcomes in Patients With Alcohol-Related Liver Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Wexner Medical Center, Columbus, OH
Introduction: Alcohol related liver disease affects diverse communities with individual and social characteristics that can impact outcomes. The Social Vulnerability Index (SVI) integrates a range of metrics and assigns a score between 0 and 1, where higher scores represent an increased risk of social vulnerability. Vulnerable patients with alcohol related liver disease have been reported to have worse outcomes. We sought to assess the impact of SVI on outcomes of patients hospitalized with alcohol related liver disease with access to social support services.
Methods: Hospitalizations for alcohol related liver disease at our institution between March and August 2019 were reviewed. All patients were assigned a low or high SVI score based on their residential census tract. Per our standard practice, patients were screened by multi-disciplinary care coordinators to identify needs for rehabilitation counseling, transplant workup, and care coordination after discharge. Demographics, hepatic decompensation, critical care needs, readmission and mortality were compared.
Results: Among 73 patients admitted for alcoholic hepatitis, 32 had a low SVI (mean 0.25) and 42 had a high SVI (mean 0.72). African American patients were more likely to have a higher SVI (35% vs 0%, p=< 0.001). Severity of alcohol hepatitis based on discriminant factor (DF) was similar between high and low SVI patients (mean DF 39.6 vs 42.8, p=0.72). After controlling for race, there was not a significant difference in hepatic decompensation, critical care needs, readmission rate or mortality based on SVI.
There were 393 patients admitted for alcoholic cirrhosis including 166 with a low SVI (mean 0.26) and 227 with a high SVI (mean 0.73). Patients that were African American (23.6% vs 5.5%, p=< 0.001) or disabled (41.4% vs 29.5%, p=0.008) had a higher SVI. MELD-Na scores were similar between the high and low SVI patients (mean MELD-Na 21.7 vs 22.9, p=0.47). After controlling for age, race and employment, there was not a significant difference in hepatic decompensation, critical care needs, readmission rate or mortality based on SVI.
Discussion: Most patients admitted for alcohol related liver disease had a high SVI; however, SVI did not impact outcomes in our cohort of patients. This may be a result of extensive care coordination efforts at our institution aimed at reducing barriers for vulnerable patients. These early interventions likely decrease the effect of SVI on outcomes.
Disclosures:
Ayushi Jain indicated no relevant financial relationships.
Michael Wellner indicated no relevant financial relationships.
Jing Peng indicated no relevant financial relationships.
Jianing Ma indicated no relevant financial relationships.
Kenneth Allen indicated no relevant financial relationships.
Chelsey McShane indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Sajid Jalil indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Sean Kelly indicated no relevant financial relationships.
Lanla Conteh indicated no relevant financial relationships.
Robert Kirkpatrick indicated no relevant financial relationships.
Lindsay Sobotka indicated no relevant financial relationships.
Ayushi Jain, MD1, Michael Wellner, MD1, Jing Peng, PhD1, Jianing Ma, PhD1, Kenneth D. Allen, MD1, Chelsey McShane, MD1, Mitchell L. Ramsey, MD1, Sajid Jalil, MBBS1, Khalid Mumtaz, MBBS, MSc2, Sean G. Kelly, MD1, Lanla F. Conteh, MD, MPH, MBA1, Robert Kirkpatrick, MD1, Lindsay A. Sobotka, DO1. E0494 - Impact of Social Vulnerability Index on Outcomes in Patients With Alcohol-Related Liver Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
