Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0530 - An Unusual Suspect in a Case of Severe Hyperammonemia
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- JY
James Yang, MD
University of Illinois
Chicago, IL
Presenting Author(s)
James Yang, MD1, Rohit Agrawal, MD1, Saul E. Turcios Escobar, MD2, Michael Stone, MD1, Adam Mikolajczyk, MD3
1University of Illinois, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3University of Illinois Medical Center, Chicago, IL
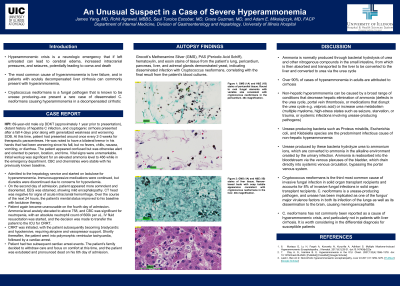
Introduction: Severe hyperammonemia is a life-threatening condition that can cause catastrophic neurologic complications from cerebral edema. Liver dysfunction is the most common etiology, but urease-producing infections are an uncommon cause. We present a rare case of severe hyperammonemia from disseminated Cryptococcus neoformans.
Case Description/Methods: A 69-year-old male with compensated cryptogenic cirrhosis who received a kidney transplant 1 year prior presented with confusion and a 30 kg weight loss. Examination revealed a scaphoid abdomen, a pericardial knock, and asterixis. Laboratory tests revealed stable kidney function (BUN 37 mg/dL, creatinine 2.3 mg/dL), mild elevation in alkaline phosphastase (204 U/L), normal albumin (3.8 g/dL) and prothrombin time (14.2 seconds), and an elevated venous ammonia level (466 mcg/dL). Serum carnitine, protein electrophoeresis, urine culture, and serum/urine amino acid analyses were normal. Magnetic resonance imaging revealed no large portosytemic shunts. Echocardiogram revealed a septal bounce in diastole consistent with constrictive physiology.
The patient was started on lactulose, rifaximin, and antimicrobial therapy with improvement in his mentation. However, on the third hospital day, the patient became obtunded. Arterial ammonia level was 758 mcg/dL. Continuous renal replacement therapy was initiated, but shortly thereafter he developed anisocoria and cardiac arrest. CT head revealed marked cerebral edema without herniation, and comfort care was then pursued. A subsequent autopsy revealed disseminated Cryptococcus neoformans infection involving the lungs, pericardium, pancreas, liver, and adrenal glands.
Discussion: Hyperammonemia results from 1) diminished metabolism to urea in the liver due to hepatocellular dysfunction, an enzymatic defect, or portosystemic shunting; 2) increased production; and/or 3) decreased excretion in kidneys or muscles. Certain organisms (e.g. Proteus) express urease, which catalyzes the hydrolysis of urea to carbon dioxide and ammonia, and can cause increased production of ammonia. Cryptococcus neoformans is a less recognized urease-producing organism and was the major source of ammonia production in our patient (coupled with impaired metabolism and excretion from cirrhosis and sarcopenia/kidney disease, respectively). Gastroenterologists need to be aware of Cryptococcus neoformans as an etiology of hyperammonemia, particularly in immunosuppressed patients unresponsive to standard therapy.
Disclosures:
James Yang, MD1, Rohit Agrawal, MD1, Saul E. Turcios Escobar, MD2, Michael Stone, MD1, Adam Mikolajczyk, MD3. E0530 - An Unusual Suspect in a Case of Severe Hyperammonemia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Illinois, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3University of Illinois Medical Center, Chicago, IL
Introduction: Severe hyperammonemia is a life-threatening condition that can cause catastrophic neurologic complications from cerebral edema. Liver dysfunction is the most common etiology, but urease-producing infections are an uncommon cause. We present a rare case of severe hyperammonemia from disseminated Cryptococcus neoformans.
Case Description/Methods: A 69-year-old male with compensated cryptogenic cirrhosis who received a kidney transplant 1 year prior presented with confusion and a 30 kg weight loss. Examination revealed a scaphoid abdomen, a pericardial knock, and asterixis. Laboratory tests revealed stable kidney function (BUN 37 mg/dL, creatinine 2.3 mg/dL), mild elevation in alkaline phosphastase (204 U/L), normal albumin (3.8 g/dL) and prothrombin time (14.2 seconds), and an elevated venous ammonia level (466 mcg/dL). Serum carnitine, protein electrophoeresis, urine culture, and serum/urine amino acid analyses were normal. Magnetic resonance imaging revealed no large portosytemic shunts. Echocardiogram revealed a septal bounce in diastole consistent with constrictive physiology.
The patient was started on lactulose, rifaximin, and antimicrobial therapy with improvement in his mentation. However, on the third hospital day, the patient became obtunded. Arterial ammonia level was 758 mcg/dL. Continuous renal replacement therapy was initiated, but shortly thereafter he developed anisocoria and cardiac arrest. CT head revealed marked cerebral edema without herniation, and comfort care was then pursued. A subsequent autopsy revealed disseminated Cryptococcus neoformans infection involving the lungs, pericardium, pancreas, liver, and adrenal glands.
Discussion: Hyperammonemia results from 1) diminished metabolism to urea in the liver due to hepatocellular dysfunction, an enzymatic defect, or portosystemic shunting; 2) increased production; and/or 3) decreased excretion in kidneys or muscles. Certain organisms (e.g. Proteus) express urease, which catalyzes the hydrolysis of urea to carbon dioxide and ammonia, and can cause increased production of ammonia. Cryptococcus neoformans is a less recognized urease-producing organism and was the major source of ammonia production in our patient (coupled with impaired metabolism and excretion from cirrhosis and sarcopenia/kidney disease, respectively). Gastroenterologists need to be aware of Cryptococcus neoformans as an etiology of hyperammonemia, particularly in immunosuppressed patients unresponsive to standard therapy.
Disclosures:
James Yang indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Saul Turcios Escobar indicated no relevant financial relationships.
Michael Stone indicated no relevant financial relationships.
Adam Mikolajczyk indicated no relevant financial relationships.
James Yang, MD1, Rohit Agrawal, MD1, Saul E. Turcios Escobar, MD2, Michael Stone, MD1, Adam Mikolajczyk, MD3. E0530 - An Unusual Suspect in a Case of Severe Hyperammonemia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
