Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0542 - Extensive Portomesenteric Venous Thrombosis Due to JAK2 V617F Mutation as an Indication for Multivisceral Transplantation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Megan B. Ghai, MD, MPH, MA
University of Arizona College of Medicine, Banner University Medical Center
Phoenix, AZ
Presenting Author(s)
Megan B. Ghai, MD, MPH, MA1, Kaelin Bernier, DO2, Mahmoud Bayoumi, MD, MPH3, Lise Harper, MD1, Rohit Nathan, DO3
1University of Arizona College of Medicine, Banner University Medical Center, Phoenix, AZ; 2UACOM-P, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, AZ
Introduction: Cavernous transformation of the portal vein (CTPV) involving periportal or intrahepatic venous collateral network is a sequelae of chronic portal vein thrombosis (PVT). This adaptation increases the risk of complications and poor outcomes from revascularization procedures. In cases with diffuse portomesenteric venous thrombosis, multivisceral transplantation (MT) may be indicated.
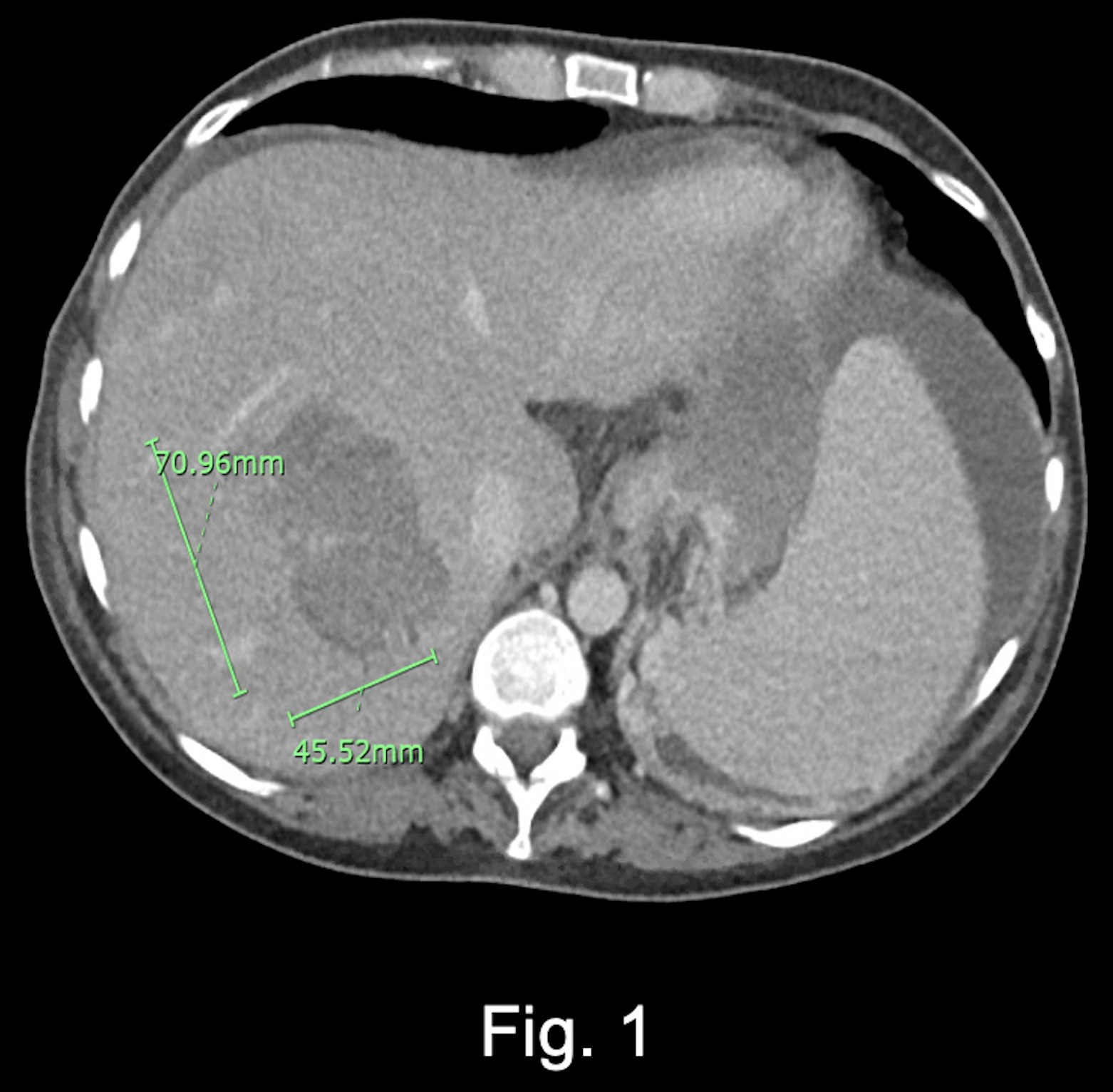
Case Description/Methods: An otherwise healthy female was diagnosed with Janus kinase 2 V617F (JAK2) mutation at age 43 during work up for PVT of unknown etiology. Her disease progressed with bleeding esophageal varices, portal hypertensive gastropathy, and splenomegaly. Liver biopsy was negative for cirrhosis. Bone marrow biopsy was negative for leukemia or fibrosis. She developed mesenteric vein thrombosis (MVT) at age 45 and was started on rivaroxaban, but then transitioned to high dose enoxaparin due to worsening thrombus progression. At age 47 she underwent thrombolysis for new MVT. Four months later, on current presentation, she endorsed worsening abdominal pain. Physical exam demonstrated ascites and pitting lower extremity edema. Abdominal ultrasound with venous duplex demonstrated absent flow in the portal vein. Computed tomography angiography (CTA) revealed progressive portal, superior mesenteric, and splenic vein thromboses despite anticoagulation (AC) compliance. Transjugular intrahepatic portosystemic shunt (TIPS) procedure was unsuccessful. Post-procedure CTA demonstrated an enlarging hepatic hematoma treated by embolization (figure 1). AC was discontinued resulting in worsening clot burden and hepatic ischemia. Given the extent of clot burden, the patient was transferred to another facility for a MT.
Discussion: Presented is a rare case of chronic PVT in a patient with JAK2 mutation leading to CTPV refractory to anticoagulation or endovascular intervention, eventually requiring MT. Though JAK2 is associated with myeloproliferative disorders, it is an independent risk factor for the development of PVT. With worsening thrombus chronicity and burden, cavernous transformation may occur which decreases the chance of successful TIPS. When organ ischemia develops due to extensive portomesenteric venous thrombosis, orthotopic liver transplantation is no longer an option. Multivisceral transplantation replaces the liver, small bowel, and other abdominal organs. Replacement of the thrombosed portomesenteric system may be the only recourse to reverse portal hypertension and address the primary disease.
Disclosures:
Megan B. Ghai, MD, MPH, MA1, Kaelin Bernier, DO2, Mahmoud Bayoumi, MD, MPH3, Lise Harper, MD1, Rohit Nathan, DO3. E0542 - Extensive Portomesenteric Venous Thrombosis Due to JAK2 V617F Mutation as an Indication for Multivisceral Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Banner University Medical Center, Phoenix, AZ; 2UACOM-P, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, AZ
Introduction: Cavernous transformation of the portal vein (CTPV) involving periportal or intrahepatic venous collateral network is a sequelae of chronic portal vein thrombosis (PVT). This adaptation increases the risk of complications and poor outcomes from revascularization procedures. In cases with diffuse portomesenteric venous thrombosis, multivisceral transplantation (MT) may be indicated.
Case Description/Methods: An otherwise healthy female was diagnosed with Janus kinase 2 V617F (JAK2) mutation at age 43 during work up for PVT of unknown etiology. Her disease progressed with bleeding esophageal varices, portal hypertensive gastropathy, and splenomegaly. Liver biopsy was negative for cirrhosis. Bone marrow biopsy was negative for leukemia or fibrosis. She developed mesenteric vein thrombosis (MVT) at age 45 and was started on rivaroxaban, but then transitioned to high dose enoxaparin due to worsening thrombus progression. At age 47 she underwent thrombolysis for new MVT. Four months later, on current presentation, she endorsed worsening abdominal pain. Physical exam demonstrated ascites and pitting lower extremity edema. Abdominal ultrasound with venous duplex demonstrated absent flow in the portal vein. Computed tomography angiography (CTA) revealed progressive portal, superior mesenteric, and splenic vein thromboses despite anticoagulation (AC) compliance. Transjugular intrahepatic portosystemic shunt (TIPS) procedure was unsuccessful. Post-procedure CTA demonstrated an enlarging hepatic hematoma treated by embolization (figure 1). AC was discontinued resulting in worsening clot burden and hepatic ischemia. Given the extent of clot burden, the patient was transferred to another facility for a MT.
Discussion: Presented is a rare case of chronic PVT in a patient with JAK2 mutation leading to CTPV refractory to anticoagulation or endovascular intervention, eventually requiring MT. Though JAK2 is associated with myeloproliferative disorders, it is an independent risk factor for the development of PVT. With worsening thrombus chronicity and burden, cavernous transformation may occur which decreases the chance of successful TIPS. When organ ischemia develops due to extensive portomesenteric venous thrombosis, orthotopic liver transplantation is no longer an option. Multivisceral transplantation replaces the liver, small bowel, and other abdominal organs. Replacement of the thrombosed portomesenteric system may be the only recourse to reverse portal hypertension and address the primary disease.
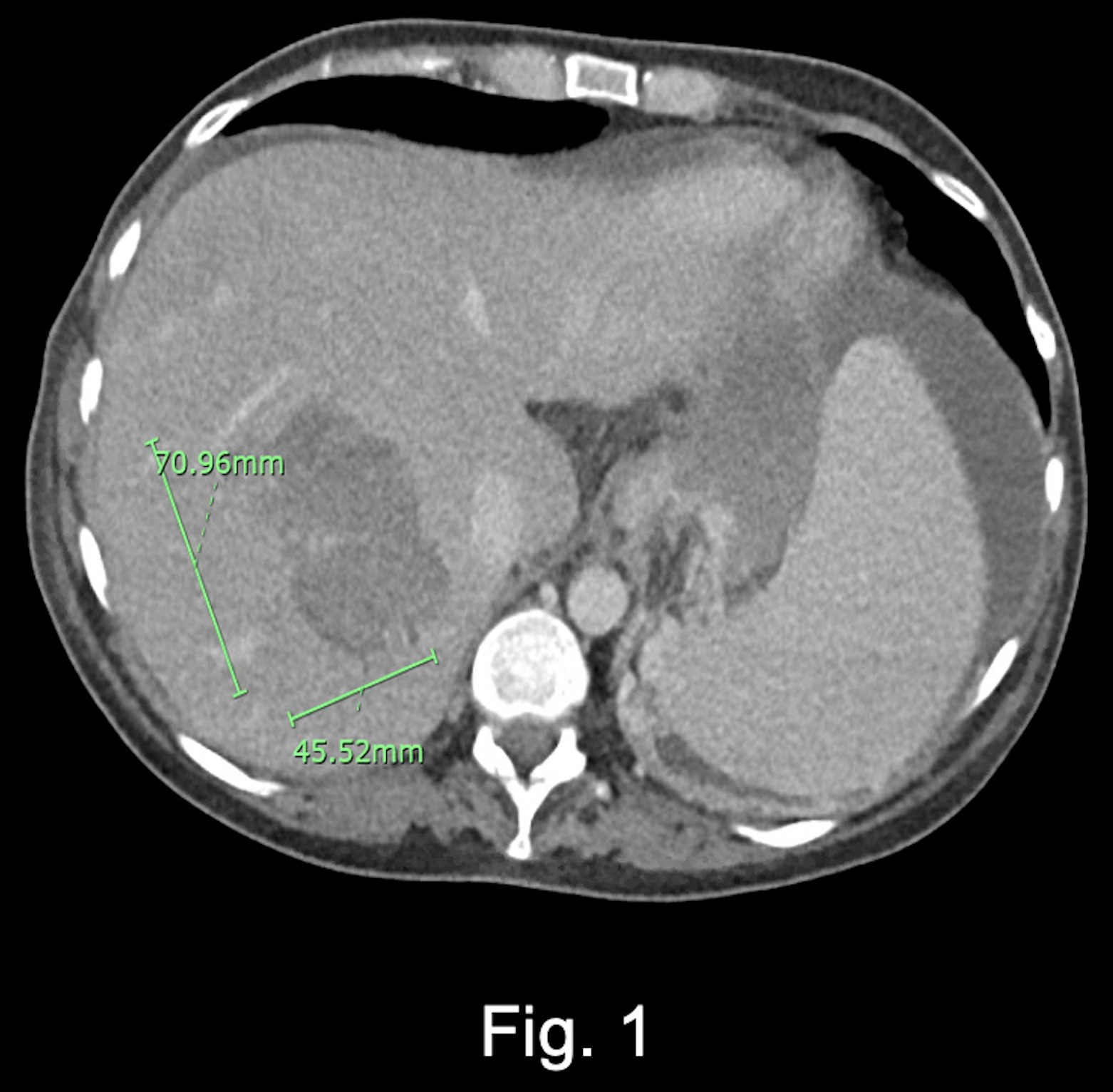
Figure: Figure 1. Computed tomography angiography of hematoma in liver segments VII and VIII, demarcated by green lines. A complication from attempted portal vein access.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Kaelin Bernier indicated no relevant financial relationships.
Mahmoud Bayoumi indicated no relevant financial relationships.
Lise Harper indicated no relevant financial relationships.
Rohit Nathan indicated no relevant financial relationships.
Megan B. Ghai, MD, MPH, MA1, Kaelin Bernier, DO2, Mahmoud Bayoumi, MD, MPH3, Lise Harper, MD1, Rohit Nathan, DO3. E0542 - Extensive Portomesenteric Venous Thrombosis Due to JAK2 V617F Mutation as an Indication for Multivisceral Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
