Back


Poster Session E - Tuesday Afternoon
Category: Esophagus
E0236 - The Black Esophagus: A Rare Complication of Diabetic Ketoacidosis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- RM
Ratib Mahfouz, MD
Brown University/Kent Hospital
Providence, RI
Presenting Author(s)
Ratib Mahfouz, MD
Brown University/Kent Hospital, Providence, RI
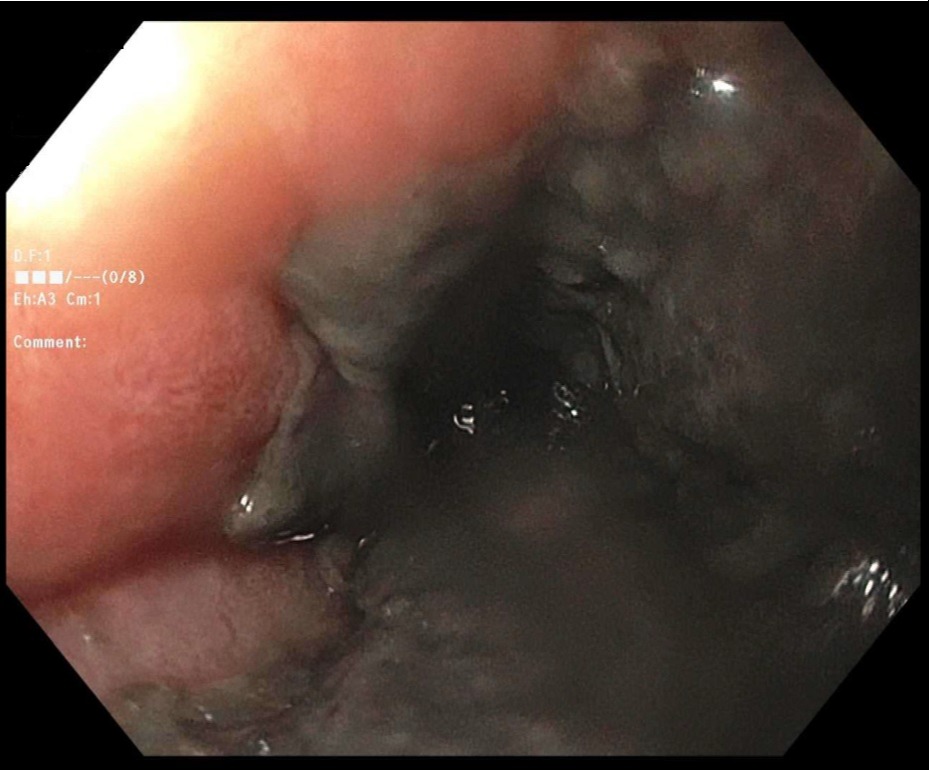
Introduction: Acute esophageal necrosis (AEN), which is also known as “black esophagus”, “acute necrotizing esophagitis”, or “Gurvits syndrome,” is a very rare condition with uncertain etiology and was first described in 1990. Its prevalence is less than 0.2%, the specific mortality is 6%, while the overall mortality rate due to comorbidities can go up to 32%. The patient is usually a male, old (average age of 67 years), and has chronic comorbidities, including cardiovascular disorders, diabetes mellitus (DM), malignancies, malnutrition, cirrhosis, gastric outlet obstruction, alcohol abuse, chronic respiratory disease, hypercoagulable state, and renal disease.
Case Description/Methods: Our patient is a 58-year-old gentleman with a past medical history of uncontrolled DM, untreated hepatitis C, and EtOH abuse disorder who was admitted to a hospital for generalized weakness and was found to have DKA. He was treated in MICU with subsequent closure of his anion gap. Later, he developed a cold foot concerning for ischemia. Computed tomography (CT) demonstrated left common femoral and popliteal artery thrombosis. He was started on heparin and underwent four-compartment fasciotomy, popliteal arteriotomy, and subsequent below-knee amputation. Later, he developed melena and hematemesis and became hemodynamically unstable with an Hgb drop down to 5.8. He had a cardiac arrest, underwent cardiopulmonary resuscitation, was intubated, and achieved a return of spontaneous circulation (ROSC). After stabilization, He underwent an EGD which showed a black esophagus consistent with the severely necrotic esophagus. He underwent bronchoscopy on the same day with no signs of tracheoesophageal fistula but was started on Micafungin due to the high risk of esophageal perforation. Sedation was weaned but remained unresponsive or able to follow commands. He was taken for a pan-scan due to worsening shock and abdominal distention, but while in the scanner, he aspirated and died.
Discussion: Researchers have proposed a "two-hit" hypothesis for AEN while the initial event is usually an ischemic state on top of an altered mucosal barrier system in a malnourished and debilitated patient. It has also been linked to backflow injury from the chemical contents of gastric secretions and thromboembolic events. Early detection is vital to preventing life-threatening complications of AEN, such as esophageal perforation and mediastinitis.
Disclosures:
Ratib Mahfouz, MD. E0236 - The Black Esophagus: A Rare Complication of Diabetic Ketoacidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Brown University/Kent Hospital, Providence, RI
Introduction: Acute esophageal necrosis (AEN), which is also known as “black esophagus”, “acute necrotizing esophagitis”, or “Gurvits syndrome,” is a very rare condition with uncertain etiology and was first described in 1990. Its prevalence is less than 0.2%, the specific mortality is 6%, while the overall mortality rate due to comorbidities can go up to 32%. The patient is usually a male, old (average age of 67 years), and has chronic comorbidities, including cardiovascular disorders, diabetes mellitus (DM), malignancies, malnutrition, cirrhosis, gastric outlet obstruction, alcohol abuse, chronic respiratory disease, hypercoagulable state, and renal disease.
Case Description/Methods: Our patient is a 58-year-old gentleman with a past medical history of uncontrolled DM, untreated hepatitis C, and EtOH abuse disorder who was admitted to a hospital for generalized weakness and was found to have DKA. He was treated in MICU with subsequent closure of his anion gap. Later, he developed a cold foot concerning for ischemia. Computed tomography (CT) demonstrated left common femoral and popliteal artery thrombosis. He was started on heparin and underwent four-compartment fasciotomy, popliteal arteriotomy, and subsequent below-knee amputation. Later, he developed melena and hematemesis and became hemodynamically unstable with an Hgb drop down to 5.8. He had a cardiac arrest, underwent cardiopulmonary resuscitation, was intubated, and achieved a return of spontaneous circulation (ROSC). After stabilization, He underwent an EGD which showed a black esophagus consistent with the severely necrotic esophagus. He underwent bronchoscopy on the same day with no signs of tracheoesophageal fistula but was started on Micafungin due to the high risk of esophageal perforation. Sedation was weaned but remained unresponsive or able to follow commands. He was taken for a pan-scan due to worsening shock and abdominal distention, but while in the scanner, he aspirated and died.
Discussion: Researchers have proposed a "two-hit" hypothesis for AEN while the initial event is usually an ischemic state on top of an altered mucosal barrier system in a malnourished and debilitated patient. It has also been linked to backflow injury from the chemical contents of gastric secretions and thromboembolic events. Early detection is vital to preventing life-threatening complications of AEN, such as esophageal perforation and mediastinitis.
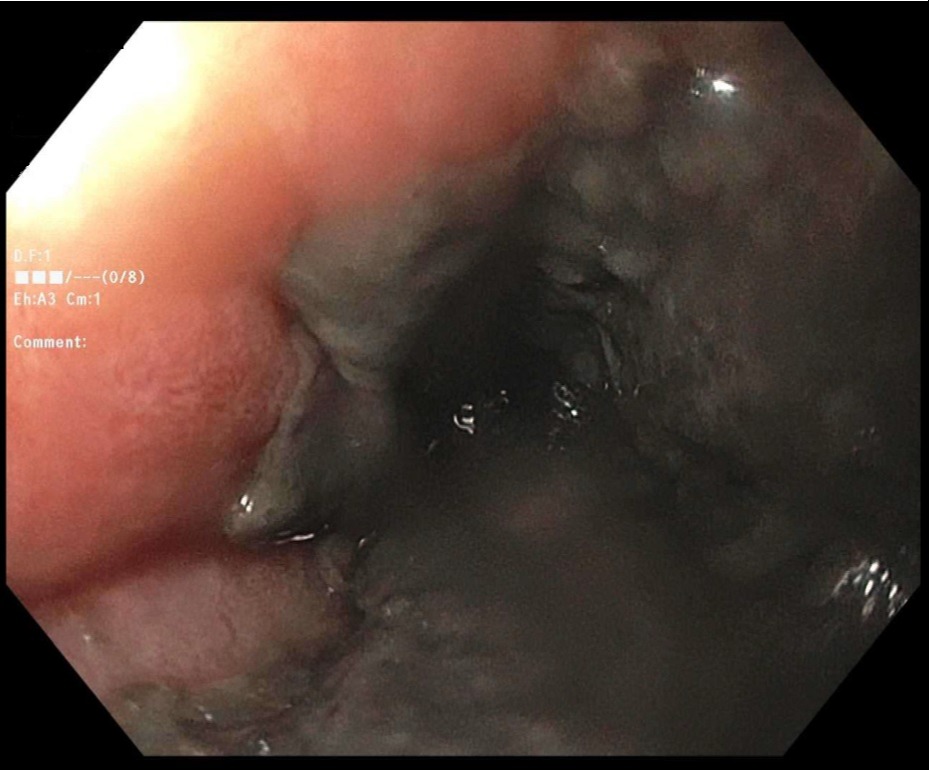
Figure: Acute esophageal necrosis
Disclosures:
Ratib Mahfouz indicated no relevant financial relationships.
Ratib Mahfouz, MD. E0236 - The Black Esophagus: A Rare Complication of Diabetic Ketoacidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
