Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0082 - Spontaneous Gastro-pancreatic Fistula: A Rare Complication of Acute Pancreatitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Ashik Pokharel, MBBS
MedStar Health
Baltimore, MD
Presenting Author(s)
Ashik Pokharel, MBBS1, Mohd Amer Alsamman, MD2, Priyanka Kanth, MD, MS2
1MedStar Health, Baltimore, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Although Gastrointestinal fistula is a well-recognized complication of acute pancreatitis, it has been rarely reported. Here we present a rare case of spontaneous gastro-pancreatic fistula following acute pancreatitis.
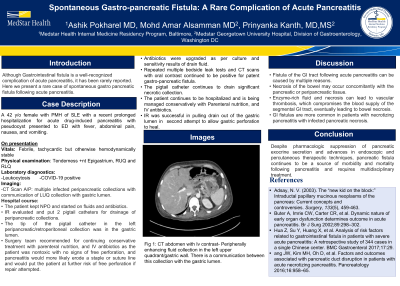
Case Description/Methods: 42 y/o female with PMH of SLE with a recent prolonged hospitalization for acute drug-induced pancreatitis with pseudocyst came to ED with fever, abdominal pain, nausea, and vomiting. She was tachycardic, had leukocytosis, and was positive for COVID-19. CT Scan A/P showed multiple infected peripancreatic collections with communication of the left upper quadrant collection with the gastric lumen. The patient was hospitalized, Kept NPO, and started on fluids and antibiotics. IR evaluated and put 2 pigtail catheters for drainage of peripancreatic collections. The tip of the pigtail catheter in the left peripancreatic/retroperitoneal collection was in the gastric lumen. The surgery team recommended continuing with conservative treatment with parenteral nutrition, and IV antibiotics as the patient were nontoxic with no signs of free perforation, and pancreatitis would more likely erode a staple or suture line and would put the patient at further risk of free perforation if repair attempted. IR was successful in pulling the drain out of the gastric lumen on the second attempt to allow gastric perforation to heal. Antibiotics were upgraded as per the culture and sensitivity results of the drain fluid. Repeated multiple bedside leak tests and CT scans with oral contrast continue to be positive for patent gastro-pancreatic fistula. Pigtails catheter continues to drain significant necrotic collection. The patient continues to be hospitalized and is being managed conservatively with Parenteral nutrition, and IV antibiotics.
Discussion:
Fistula of the GI tract following acute pancreatitis can be caused by multiple reasons. Necrosis of the bowel may occur concomitantly with the pancreatic or peripancreatic tissue. Furthermore, enzyme-rich fluid and necrosis can lead to vascular thrombosis, which compromises the blood supply of the segmental GI tract, eventually leading to bowel necrosis. GI fistulas are more common in patients with necrotizing pancreatitis with infected pancreatic necrosis. Despite pharmacologic suppression of pancreatic exocrine secretion and advances in endoscopic and percutaneous therapeutic techniques, pancreatic fistula continues to be a source of morbidity and mortality following pancreatitis and requires multidisciplinary treatment.

Disclosures:
Ashik Pokharel, MBBS1, Mohd Amer Alsamman, MD2, Priyanka Kanth, MD, MS2. A0082 - Spontaneous Gastro-pancreatic Fistula: A Rare Complication of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1MedStar Health, Baltimore, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Although Gastrointestinal fistula is a well-recognized complication of acute pancreatitis, it has been rarely reported. Here we present a rare case of spontaneous gastro-pancreatic fistula following acute pancreatitis.
Case Description/Methods: 42 y/o female with PMH of SLE with a recent prolonged hospitalization for acute drug-induced pancreatitis with pseudocyst came to ED with fever, abdominal pain, nausea, and vomiting. She was tachycardic, had leukocytosis, and was positive for COVID-19. CT Scan A/P showed multiple infected peripancreatic collections with communication of the left upper quadrant collection with the gastric lumen. The patient was hospitalized, Kept NPO, and started on fluids and antibiotics. IR evaluated and put 2 pigtail catheters for drainage of peripancreatic collections. The tip of the pigtail catheter in the left peripancreatic/retroperitoneal collection was in the gastric lumen. The surgery team recommended continuing with conservative treatment with parenteral nutrition, and IV antibiotics as the patient were nontoxic with no signs of free perforation, and pancreatitis would more likely erode a staple or suture line and would put the patient at further risk of free perforation if repair attempted. IR was successful in pulling the drain out of the gastric lumen on the second attempt to allow gastric perforation to heal. Antibiotics were upgraded as per the culture and sensitivity results of the drain fluid. Repeated multiple bedside leak tests and CT scans with oral contrast continue to be positive for patent gastro-pancreatic fistula. Pigtails catheter continues to drain significant necrotic collection. The patient continues to be hospitalized and is being managed conservatively with Parenteral nutrition, and IV antibiotics.
Discussion:
Fistula of the GI tract following acute pancreatitis can be caused by multiple reasons. Necrosis of the bowel may occur concomitantly with the pancreatic or peripancreatic tissue. Furthermore, enzyme-rich fluid and necrosis can lead to vascular thrombosis, which compromises the blood supply of the segmental GI tract, eventually leading to bowel necrosis. GI fistulas are more common in patients with necrotizing pancreatitis with infected pancreatic necrosis. Despite pharmacologic suppression of pancreatic exocrine secretion and advances in endoscopic and percutaneous therapeutic techniques, pancreatic fistula continues to be a source of morbidity and mortality following pancreatitis and requires multidisciplinary treatment.

Figure: Peripherally enhancing fluid collection in the left upper quadrant/gastric wall. There is a communication between this collection with the gastric lumen.
Disclosures:
Ashik Pokharel indicated no relevant financial relationships.
Mohd Amer Alsamman indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Ashik Pokharel, MBBS1, Mohd Amer Alsamman, MD2, Priyanka Kanth, MD, MS2. A0082 - Spontaneous Gastro-pancreatic Fistula: A Rare Complication of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
