Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0577 - A Hare Unusual: Francisella tularensis Peritonitis Following Orthotopic Liver Transplantation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- JC
Jacob Ciricillo, MD
University of Cincinnati Medical Center
Cincinnati, OH
Presenting Author(s)
Jacob Ciricillo, MD, Alexandra N. Willauer, MD, Michael Schoech, MD
University of Cincinnati Medical Center, Cincinnati, OH
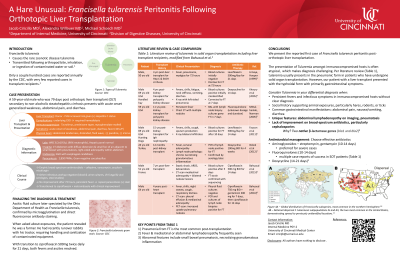
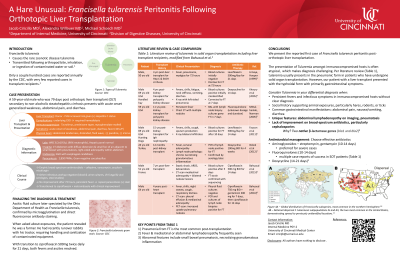
Introduction: Francisella tularensis (FT) causes the rare zoonotic disease tularemia. FT is transmitted following arthropod bite, inhalation, or ingestion of contaminated water or soil. Only a couple hundred cases are reported annually by the CDC, with few in transplant recipients. In immunocompromised hosts (ICH), the clinical manifestations may be atypical and there is limited literature on the management of FT in this population.
Case Description/Methods: A 59-year-old male who was 79 days post orthotopic liver transplant (OLT) secondary to non-alcoholic steatohepatitis cirrhosis presents with acute onset generalized weakness, abdominal pain, and diarrhea. Immunosuppression included mycophenolate mofetil and tacrolimus. He was febrile to 103.2F on admission. Physical examination revealed diffuse abdominal tenderness and distension due to ascites. Laboratory tests were notable for WBC count of 8.2x10^3/μL with 96% neutrophils and a normal hepatic panel. Imaging displayed diffuse distention of the small bowel with pneumatosis. Given the broad infectious differential in an ICH, he was empirically started on cefepime, vancomycin, metronidazole, acyclovir, and micafungin. Diagnostic paracentesis revealed peritonitis with 2,850 polymorphonuclear leukocytes and gram stain with gram-negative coccobacillus. Work-up including lumbar puncture, blood cultures, and fungal and viral serologies was negative. His fever persisted and repeat ascitic fluid was unchanged at 72 hours despite empiric treatment. Ascitic fluid culture later speciated as FT confirmed with microagglutination and direct fluorescence antibody staining. When asked about exposures, the patient revealed he was a farmer and had recently runover rabbits with his tractor, requiring handling and sanitization of contaminated equipment. With transition to ciprofloxacin 500mg twice daily for 21 days, both fevers and ascites resolved.
Discussion: To our knowledge, this is the first case of FT peritonitis reported post-OLT and the third case of tularemia post-liver transplant. Our patient likely inhaled bacteria from contaminated soil or after handling infected rabbits and experienced subsequent gut translocation. Treatment with gentamicin or streptomycin is recommended in severe FT cases and doxycycline or ciprofloxacin for mild disease. Given atypical presentation in immunosuppressed hosts, we recommend consideration of tularemia as a cause of unexplained persistent fever, ascites, or lymphadenopathy post-transplant in patients with risk of FT exposure.
Disclosures:
Jacob Ciricillo, MD, Alexandra N. Willauer, MD, Michael Schoech, MD. E0577 - A Hare Unusual: Francisella tularensis Peritonitis Following Orthotopic Liver Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Francisella tularensis (FT) causes the rare zoonotic disease tularemia. FT is transmitted following arthropod bite, inhalation, or ingestion of contaminated water or soil. Only a couple hundred cases are reported annually by the CDC, with few in transplant recipients. In immunocompromised hosts (ICH), the clinical manifestations may be atypical and there is limited literature on the management of FT in this population.
Case Description/Methods: A 59-year-old male who was 79 days post orthotopic liver transplant (OLT) secondary to non-alcoholic steatohepatitis cirrhosis presents with acute onset generalized weakness, abdominal pain, and diarrhea. Immunosuppression included mycophenolate mofetil and tacrolimus. He was febrile to 103.2F on admission. Physical examination revealed diffuse abdominal tenderness and distension due to ascites. Laboratory tests were notable for WBC count of 8.2x10^3/μL with 96% neutrophils and a normal hepatic panel. Imaging displayed diffuse distention of the small bowel with pneumatosis. Given the broad infectious differential in an ICH, he was empirically started on cefepime, vancomycin, metronidazole, acyclovir, and micafungin. Diagnostic paracentesis revealed peritonitis with 2,850 polymorphonuclear leukocytes and gram stain with gram-negative coccobacillus. Work-up including lumbar puncture, blood cultures, and fungal and viral serologies was negative. His fever persisted and repeat ascitic fluid was unchanged at 72 hours despite empiric treatment. Ascitic fluid culture later speciated as FT confirmed with microagglutination and direct fluorescence antibody staining. When asked about exposures, the patient revealed he was a farmer and had recently runover rabbits with his tractor, requiring handling and sanitization of contaminated equipment. With transition to ciprofloxacin 500mg twice daily for 21 days, both fevers and ascites resolved.
Discussion: To our knowledge, this is the first case of FT peritonitis reported post-OLT and the third case of tularemia post-liver transplant. Our patient likely inhaled bacteria from contaminated soil or after handling infected rabbits and experienced subsequent gut translocation. Treatment with gentamicin or streptomycin is recommended in severe FT cases and doxycycline or ciprofloxacin for mild disease. Given atypical presentation in immunosuppressed hosts, we recommend consideration of tularemia as a cause of unexplained persistent fever, ascites, or lymphadenopathy post-transplant in patients with risk of FT exposure.
Disclosures:
Jacob Ciricillo indicated no relevant financial relationships.
Alexandra Willauer indicated no relevant financial relationships.
Michael Schoech indicated no relevant financial relationships.
Jacob Ciricillo, MD, Alexandra N. Willauer, MD, Michael Schoech, MD. E0577 - A Hare Unusual: Francisella tularensis Peritonitis Following Orthotopic Liver Transplantation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

