Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0579 - Collapsing Alcoholic Cirrhosis Presenting as Functional Budd-Chiari Syndrome
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Joshua Diaz, MD
Coney Island Hospital
Brooklyn, NY
Presenting Author(s)
Joshua Diaz, MD, Nikolas St. Cyr, MD, Michael Bernstein, MD
Coney Island Hospital, Brooklyn, NY
Introduction: Budd-Chiari syndrome (BCS) is a rare disease involving hepatic venous obstruction, often associated with hypercoagulability. Treatment with anticoagulation (AC) and thrombolysis is imperative in BCS; however, this also carries substantial risk. Thus, additional studies are important in confirming BCS prior to initiating treatment. Here we have a case that presented similarly to BCS, but was later ruled out using ultrasonogram (US) with doppler and triphasic CT scan for confirmation, altering the management plan.
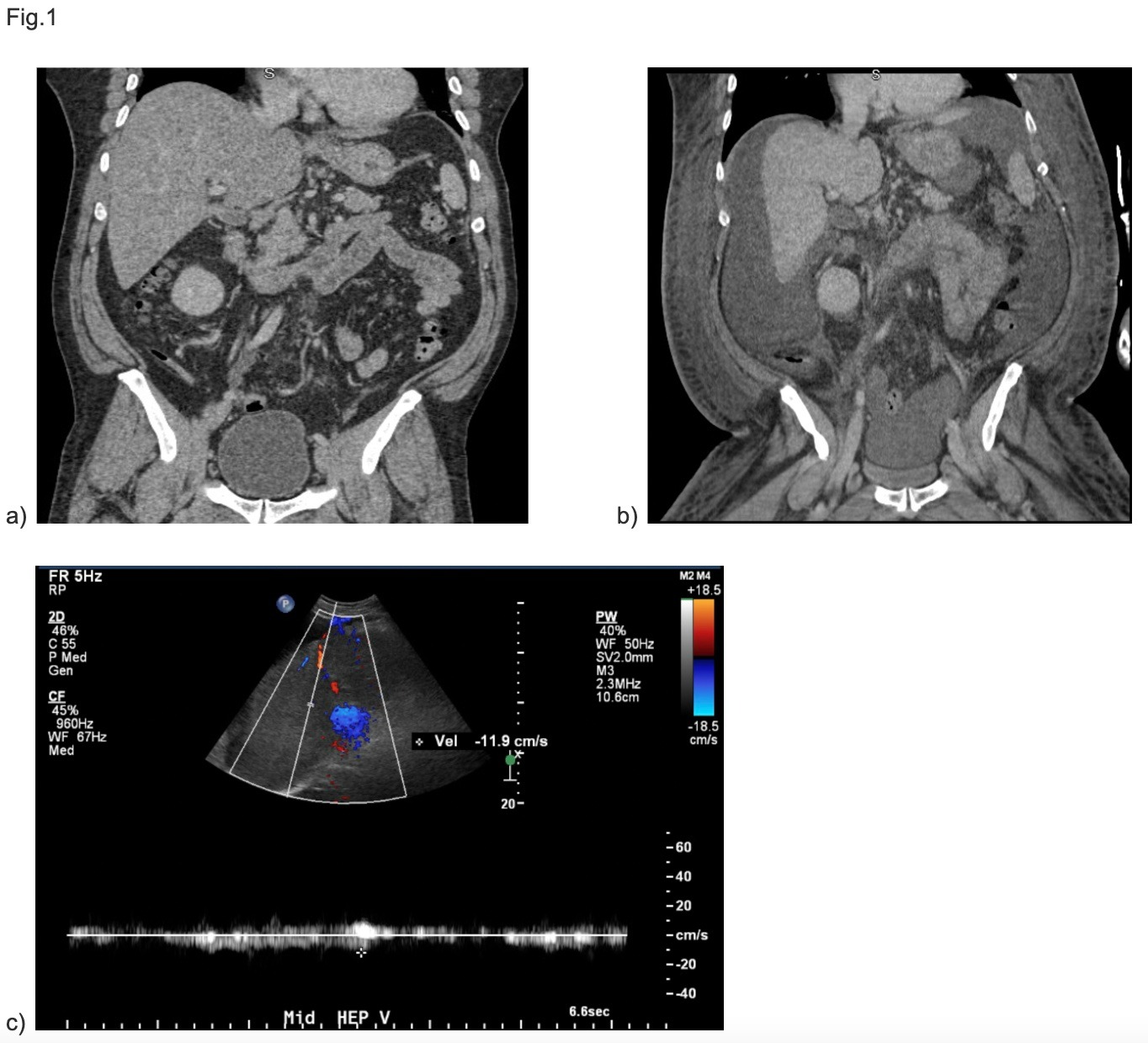
Case Description/Methods: A 49 year old male with alcoholic cirrhosis and esophageal varices presented with bilateral lower extremity edema, abdominal pain and dyspnea. Physical exam found scleral icterus, jaundice, abdominal distention with fluid wave, bilateral lower extremity edema and tenderness. Labs showed platelets of 83, ALK 268, AST 44, ALT 23, Direct bilirubin 1.4 and ammonia 48. He was admitted for decompensated liver cirrhosis and prophylaxis for spontaneous bacterial peritonitis was initiated. Patient was diuresed and underwent paracentesis. Fluid analysis showed SAAG > 1.1 and Neutrophils < 250, indicating portal hypertension. Doppler US showed attenuated caliber of hepatic veins and discontinuity between these and the IVC. Confirmatory study with Triphasic CT showed a shrunken liver without clots, ruling out primary BCS. Patient was deemed unsuitable for TIPS given MELD-Na of 20, degree of hepatic damage and transplant unavailability, and was discharged on medical management.
Discussion: This case of alcoholic cirrhosis shares clinical and physiologic similarities with BCS. Differentiating between the two is key to initiating correct intervention and minimizing complications. This patient has atrophied hepatic architecture that serves as an outflow obstruction similar to that seen in BCS. Imaging with doppler US, CT or MRI looks for direct and indirect signs of BCS; here, no diagnostic signs were observed, despite a defect of venous outflow on doppler US. Had confirmatory tests not ruled out BCS, AC likely would have been initiated, exposing him to unnecessary risks. This highlights a patient with advanced alcoholic cirrhosis presenting with signs and symptoms suspicious for BCS. Initial imaging was also concerning for BCS, but confirmatory tests proved otherwise. This illustrates the value of confirmatory triphasic CT scan in a patient with US findings that are suspicious for, but not confirmatory of, BCS, guiding treatment away from AC and its risks and complications.
Disclosures:
Joshua Diaz, MD, Nikolas St. Cyr, MD, Michael Bernstein, MD. E0579 - Collapsing Alcoholic Cirrhosis Presenting as Functional Budd-Chiari Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Coney Island Hospital, Brooklyn, NY
Introduction: Budd-Chiari syndrome (BCS) is a rare disease involving hepatic venous obstruction, often associated with hypercoagulability. Treatment with anticoagulation (AC) and thrombolysis is imperative in BCS; however, this also carries substantial risk. Thus, additional studies are important in confirming BCS prior to initiating treatment. Here we have a case that presented similarly to BCS, but was later ruled out using ultrasonogram (US) with doppler and triphasic CT scan for confirmation, altering the management plan.
Case Description/Methods: A 49 year old male with alcoholic cirrhosis and esophageal varices presented with bilateral lower extremity edema, abdominal pain and dyspnea. Physical exam found scleral icterus, jaundice, abdominal distention with fluid wave, bilateral lower extremity edema and tenderness. Labs showed platelets of 83, ALK 268, AST 44, ALT 23, Direct bilirubin 1.4 and ammonia 48. He was admitted for decompensated liver cirrhosis and prophylaxis for spontaneous bacterial peritonitis was initiated. Patient was diuresed and underwent paracentesis. Fluid analysis showed SAAG > 1.1 and Neutrophils < 250, indicating portal hypertension. Doppler US showed attenuated caliber of hepatic veins and discontinuity between these and the IVC. Confirmatory study with Triphasic CT showed a shrunken liver without clots, ruling out primary BCS. Patient was deemed unsuitable for TIPS given MELD-Na of 20, degree of hepatic damage and transplant unavailability, and was discharged on medical management.
Discussion: This case of alcoholic cirrhosis shares clinical and physiologic similarities with BCS. Differentiating between the two is key to initiating correct intervention and minimizing complications. This patient has atrophied hepatic architecture that serves as an outflow obstruction similar to that seen in BCS. Imaging with doppler US, CT or MRI looks for direct and indirect signs of BCS; here, no diagnostic signs were observed, despite a defect of venous outflow on doppler US. Had confirmatory tests not ruled out BCS, AC likely would have been initiated, exposing him to unnecessary risks. This highlights a patient with advanced alcoholic cirrhosis presenting with signs and symptoms suspicious for BCS. Initial imaging was also concerning for BCS, but confirmatory tests proved otherwise. This illustrates the value of confirmatory triphasic CT scan in a patient with US findings that are suspicious for, but not confirmatory of, BCS, guiding treatment away from AC and its risks and complications.
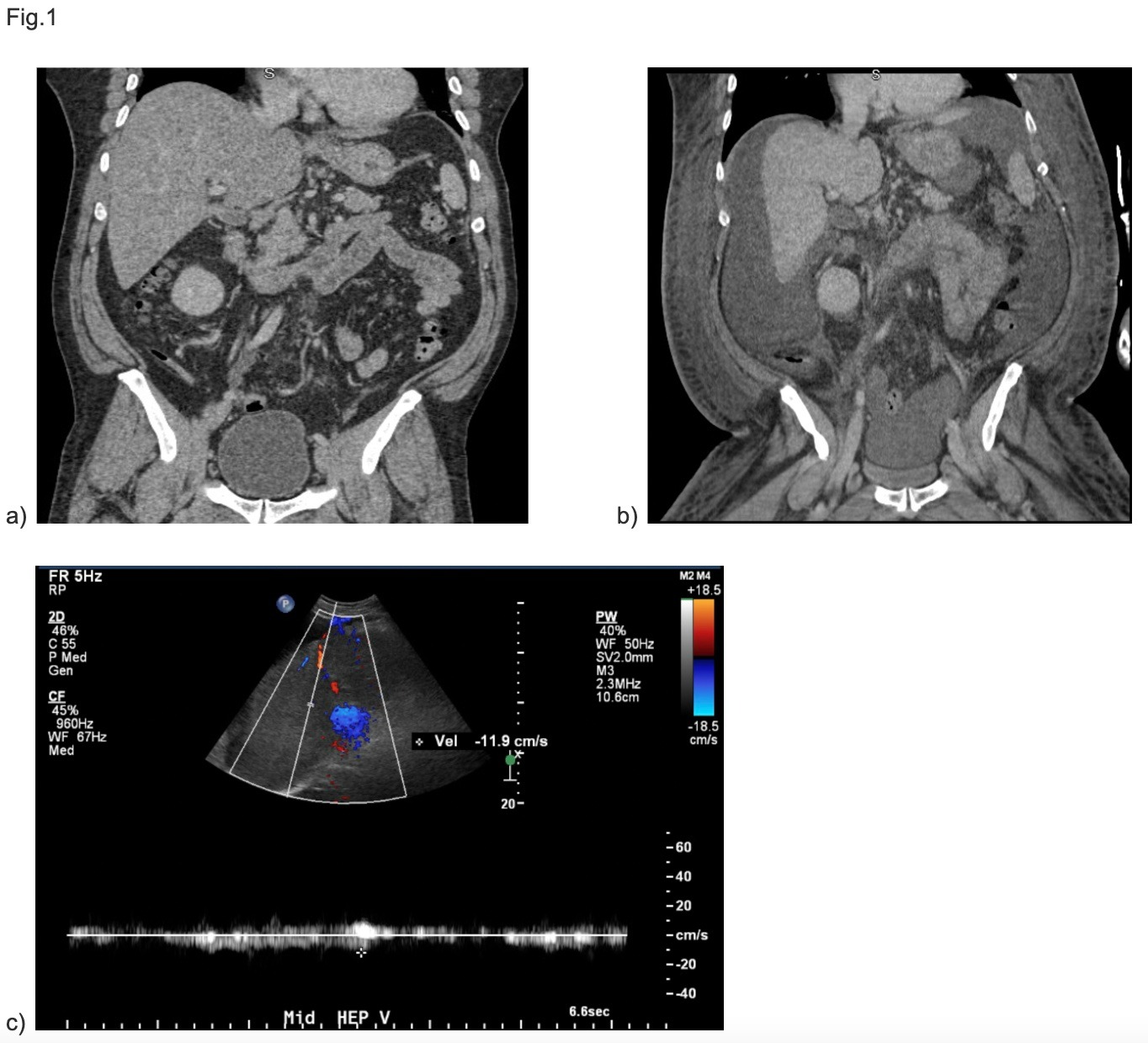
Figure: Fig. 1 (a) CT scan abdomen and pelvis illustrating hepatomegaly and nodular liver contour suggestive of cirrhosis (2019).
b) CT scan abdomen and pelvis showing significantly shrunken liver with modularity and ascites (2022)
c)US with Doppler showing attenuated middle hepatic vein with reduced flow velocity.
b) CT scan abdomen and pelvis showing significantly shrunken liver with modularity and ascites (2022)
c)US with Doppler showing attenuated middle hepatic vein with reduced flow velocity.
Disclosures:
Joshua Diaz indicated no relevant financial relationships.
Nikolas St. Cyr indicated no relevant financial relationships.
Michael Bernstein indicated no relevant financial relationships.
Joshua Diaz, MD, Nikolas St. Cyr, MD, Michael Bernstein, MD. E0579 - Collapsing Alcoholic Cirrhosis Presenting as Functional Budd-Chiari Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
