Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0587 - The Case of the Disappearing Ducts: Hodgkin’s Lymphoma Presenting With Vanishing Bile Duct Syndrome
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- JM
Judah Morgan, MD
Madigan Army Medical Center
Auburn, WA
Presenting Author(s)
Judah Morgan, MD1, Robert C. Weishar, BS2, Charles Larcom, MD3, Ryan Kwok, MD1
1Madigan Army Medical Center, Auburn, WA; 2Uniformed Services University of the Health Sciences, Bethesda, MD; 3Madigan Army Medical Center, Joint Base Lewis McCord, WA
Introduction: Classical Hodgkin’s Lymphoma (cHL) can involve hepatic dysfunction that may arise through a variety of mechanisms. These include direct infiltration, viral reactivation, bile duct obstruction, hemophagocytic proliferation, drug induced injury, and paraneoplastic phenomenon. Vanishing Bile Duct Syndrome (VBDS) is a rare, acquired condition involving destruction and loss of intrahepatic bile ducts leading to cholestasis that has been associated with various etiologies including as a paraneoplastic phenomenon associated with cHL. This is a case of a 24-year-old with VBDS ultimately found to be the cause of profound cholestatic liver injury present at the time of a new diagnosis of cHL.
Case Description/Methods: The patient presented with abdominal pain, nausea, and jaundice for 1 week as well as night sweats and weight loss for about 6 months. Physical exam was notable for marked jaundice, scleral icterus, and diffuse lymphadenopathy. Labs showed a cholestatic pattern of liver injury with a severe direct hyperbilirubinemia and mildly elevated transaminases. A lymph node biopsy demonstrated cHL and an MRCP showed hepatomegaly without biliary dilation, obstruction, or other focal abnormalities. Laboratory evaluation for metabolic, autoimmune, viral and other infectious etiologies were negative. A subsequent liver biopsy showed inflammation of the portal tracts, no lymphoproliferative infiltration, and focal small bile duct drop out consistent with VBDS. The patient was treated with prednisone, colestipol, ursodiol, and diphenhydramine for symptom management and promptly initiated on chemotherapy.
Discussion: In cases such as this, a complete evaluation is essential. A liver biopsy is required for this diagnosis and can be done while some other tests are still pending if suspicion is high enough. Overall, there have been 29 cases of this syndrome associated with HL reported in the literature since 1993. It seems that 10 of these cases, a total of 34%, resolved after successful treatment and remission of cHL. Early and aggressive treatment of the underlying malignancy is recommended in these cases which highlights the importance of recognition of this rare syndrome. Although this case highlights a particular rare entity that may cause cholestatic liver injury in patients with cHL, it is paramount to conduct a thorough evaluation for other potential causes to include infiltrative, viral, obstructive, autoimmune, and drug-induced processes.
Disclosures:
Judah Morgan, MD1, Robert C. Weishar, BS2, Charles Larcom, MD3, Ryan Kwok, MD1. E0587 - The Case of the Disappearing Ducts: Hodgkin’s Lymphoma Presenting With Vanishing Bile Duct Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Madigan Army Medical Center, Auburn, WA; 2Uniformed Services University of the Health Sciences, Bethesda, MD; 3Madigan Army Medical Center, Joint Base Lewis McCord, WA
Introduction: Classical Hodgkin’s Lymphoma (cHL) can involve hepatic dysfunction that may arise through a variety of mechanisms. These include direct infiltration, viral reactivation, bile duct obstruction, hemophagocytic proliferation, drug induced injury, and paraneoplastic phenomenon. Vanishing Bile Duct Syndrome (VBDS) is a rare, acquired condition involving destruction and loss of intrahepatic bile ducts leading to cholestasis that has been associated with various etiologies including as a paraneoplastic phenomenon associated with cHL. This is a case of a 24-year-old with VBDS ultimately found to be the cause of profound cholestatic liver injury present at the time of a new diagnosis of cHL.
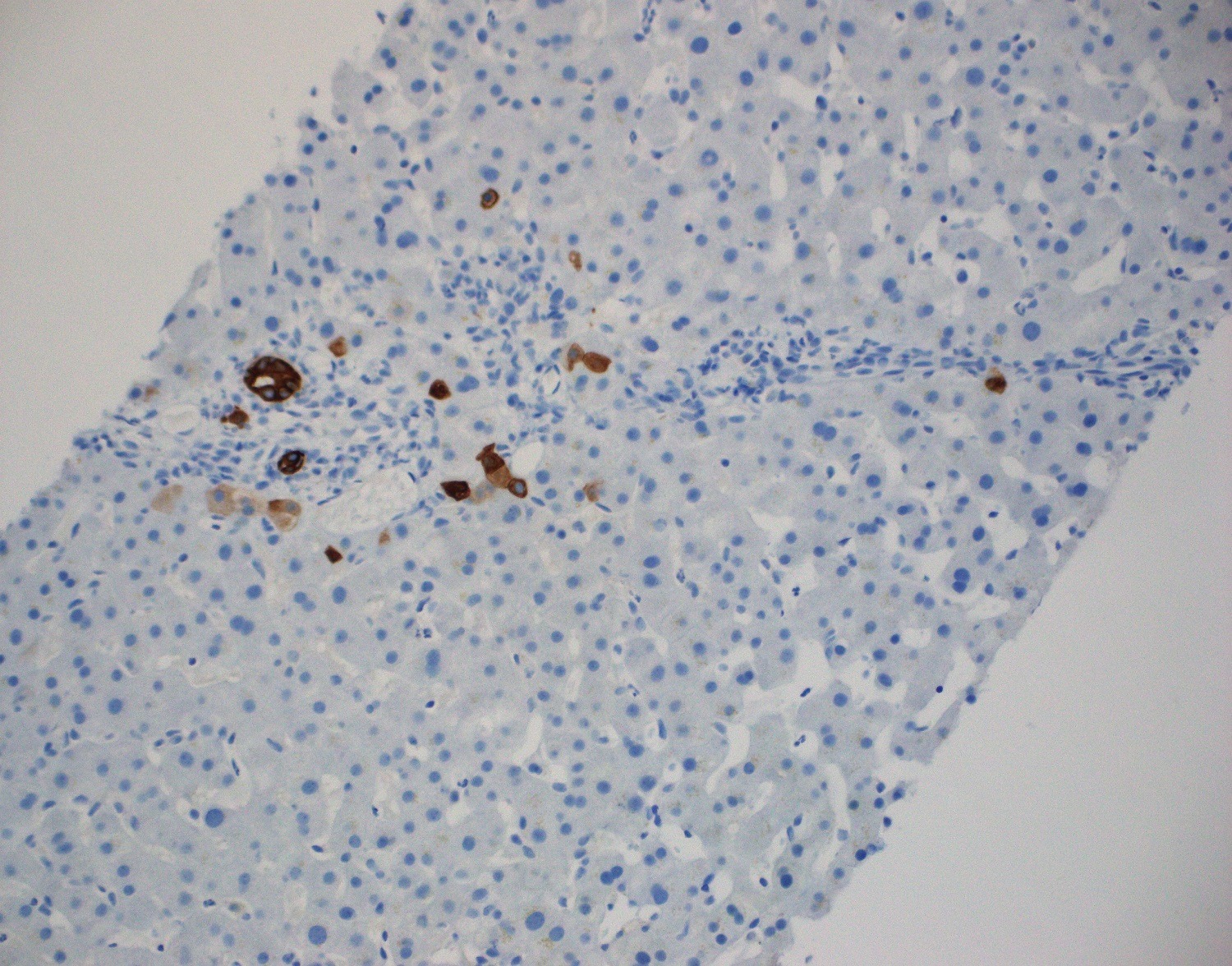
Case Description/Methods: The patient presented with abdominal pain, nausea, and jaundice for 1 week as well as night sweats and weight loss for about 6 months. Physical exam was notable for marked jaundice, scleral icterus, and diffuse lymphadenopathy. Labs showed a cholestatic pattern of liver injury with a severe direct hyperbilirubinemia and mildly elevated transaminases. A lymph node biopsy demonstrated cHL and an MRCP showed hepatomegaly without biliary dilation, obstruction, or other focal abnormalities. Laboratory evaluation for metabolic, autoimmune, viral and other infectious etiologies were negative. A subsequent liver biopsy showed inflammation of the portal tracts, no lymphoproliferative infiltration, and focal small bile duct drop out consistent with VBDS. The patient was treated with prednisone, colestipol, ursodiol, and diphenhydramine for symptom management and promptly initiated on chemotherapy.
Discussion: In cases such as this, a complete evaluation is essential. A liver biopsy is required for this diagnosis and can be done while some other tests are still pending if suspicion is high enough. Overall, there have been 29 cases of this syndrome associated with HL reported in the literature since 1993. It seems that 10 of these cases, a total of 34%, resolved after successful treatment and remission of cHL. Early and aggressive treatment of the underlying malignancy is recommended in these cases which highlights the importance of recognition of this rare syndrome. Although this case highlights a particular rare entity that may cause cholestatic liver injury in patients with cHL, it is paramount to conduct a thorough evaluation for other potential causes to include infiltrative, viral, obstructive, autoimmune, and drug-induced processes.
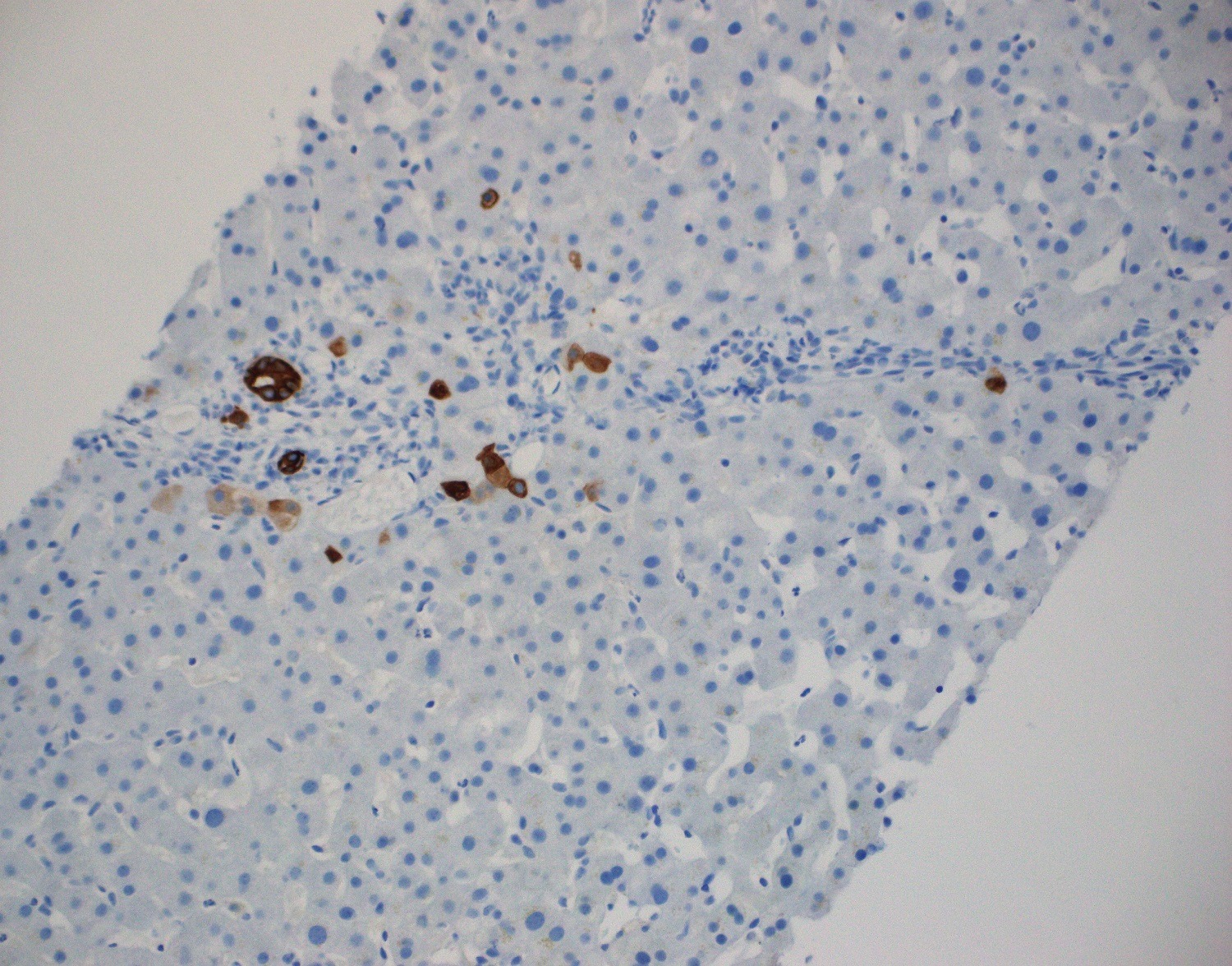
Figure: Liver Biopsy with IHC stain for CK7 showing disrupted small bile ducts and small duct proliferation
Disclosures:
Judah Morgan indicated no relevant financial relationships.
Robert Weishar indicated no relevant financial relationships.
Charles Larcom indicated no relevant financial relationships.
Ryan Kwok indicated no relevant financial relationships.
Judah Morgan, MD1, Robert C. Weishar, BS2, Charles Larcom, MD3, Ryan Kwok, MD1. E0587 - The Case of the Disappearing Ducts: Hodgkin’s Lymphoma Presenting With Vanishing Bile Duct Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
