Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0588 - A Case of Isolated Hepatic Tuberculosis in an Immunocompromised Patient
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- IF
Irtiqa Fazili, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Irtiqa Fazili, MD, Cindy Ye, MD, Emad Qayed, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Primary hepatic tuberculosis is a rare clinical entity with non-specific clinical and imaging features that can mimic other liver diseases, presenting a diagnostic challenge. We present a case of a patient with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) who developed fevers of unknown origin and elevated liver enzymes. Liver biopsy was key to diagnosis as it revealed necrotizing granulomas consistent with tuberculous hepatitis.
Case Description/Methods: The patient is a 54-year-old female with uncontrolled HIV/AIDS (CD4 6/1%) who presented with fever, encephalopathy, and abdominal pain. She was febrile to 38, tachycardic to 103, blood pressure 144/115, 96% on room air. She was ill-appearing, altered, nonverbal, with epigastric and lower abdominal tenderness on exam. Complete metabolic panel, complete blood count, lipase, and lactic acid were all within normal limits on presentation. CT of the abdomen and pelvis was unrevealing.
On admission, she was found to have community acquired pneumonia, a urinary tract infection, a pulmonary embolism, and HIV-associated neurocognitive disorder. She was started on antiretrovirals and improved until she developed fevers of unknown origin and newly elevated liver enzymes (aspartate transaminase 400s, alanine aminotransferase 300s, alkaline phosphatase 1200s, total bilirubin 12.4, direct bilirubin 7.1) over the course of her prolonged hospitalization. A hepatic workup was largely unrevealing for etiology. Hepatitis panel, drug panel, cytomegalovirus, and Epstein-Barr virus were all negative. Autoimmune workup was weakly positive for anti-nuclear and anti-smooth muscle antibodies, but these were felt to be clinically insignificant due to low titers. The patient was also trialed on intravenous steroids with little improvement, further arguing against the diagnosis of autoimmune hepatitis. Liver biopsy revealed lobular necrotizing granulomas with scattered histiocytes and lymphocytes, consistent with tuberculous granulomatous hepatitis. She started tuberculosis therapy and tolerated it well.
Discussion: Primary hepatic tuberculosis with no clinical extrahepatic manifestations is a rare presentation and sporadically reported in the literature. This clinical case highlights the diagnostic difficulty of hepatic tuberculosis, which should be considered in immunocompromised patients with elevated liver enzymes and unrevealing initial workup. Liver biopsy is essential for diagnosis.
Disclosures:
Irtiqa Fazili, MD, Cindy Ye, MD, Emad Qayed, MD. E0588 - A Case of Isolated Hepatic Tuberculosis in an Immunocompromised Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Primary hepatic tuberculosis is a rare clinical entity with non-specific clinical and imaging features that can mimic other liver diseases, presenting a diagnostic challenge. We present a case of a patient with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) who developed fevers of unknown origin and elevated liver enzymes. Liver biopsy was key to diagnosis as it revealed necrotizing granulomas consistent with tuberculous hepatitis.
Case Description/Methods: The patient is a 54-year-old female with uncontrolled HIV/AIDS (CD4 6/1%) who presented with fever, encephalopathy, and abdominal pain. She was febrile to 38, tachycardic to 103, blood pressure 144/115, 96% on room air. She was ill-appearing, altered, nonverbal, with epigastric and lower abdominal tenderness on exam. Complete metabolic panel, complete blood count, lipase, and lactic acid were all within normal limits on presentation. CT of the abdomen and pelvis was unrevealing.
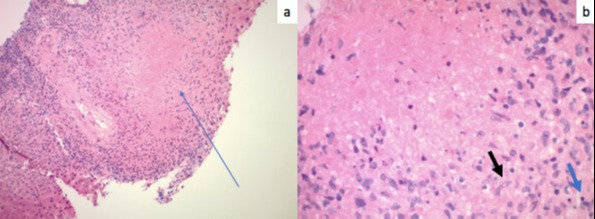
On admission, she was found to have community acquired pneumonia, a urinary tract infection, a pulmonary embolism, and HIV-associated neurocognitive disorder. She was started on antiretrovirals and improved until she developed fevers of unknown origin and newly elevated liver enzymes (aspartate transaminase 400s, alanine aminotransferase 300s, alkaline phosphatase 1200s, total bilirubin 12.4, direct bilirubin 7.1) over the course of her prolonged hospitalization. A hepatic workup was largely unrevealing for etiology. Hepatitis panel, drug panel, cytomegalovirus, and Epstein-Barr virus were all negative. Autoimmune workup was weakly positive for anti-nuclear and anti-smooth muscle antibodies, but these were felt to be clinically insignificant due to low titers. The patient was also trialed on intravenous steroids with little improvement, further arguing against the diagnosis of autoimmune hepatitis. Liver biopsy revealed lobular necrotizing granulomas with scattered histiocytes and lymphocytes, consistent with tuberculous granulomatous hepatitis. She started tuberculosis therapy and tolerated it well.
Discussion: Primary hepatic tuberculosis with no clinical extrahepatic manifestations is a rare presentation and sporadically reported in the literature. This clinical case highlights the diagnostic difficulty of hepatic tuberculosis, which should be considered in immunocompromised patients with elevated liver enzymes and unrevealing initial workup. Liver biopsy is essential for diagnosis.
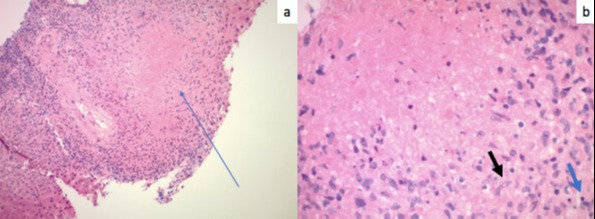
Figure: a) Lobular necrotizing granuloma; b) Center of necrotizing granuloma with histiocytes (black arrow) and lymphocytes (blue arrow)
Disclosures:
Irtiqa Fazili indicated no relevant financial relationships.
Cindy Ye indicated no relevant financial relationships.
Emad Qayed indicated no relevant financial relationships.
Irtiqa Fazili, MD, Cindy Ye, MD, Emad Qayed, MD. E0588 - A Case of Isolated Hepatic Tuberculosis in an Immunocompromised Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
