Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0592 - Esophageal Varices in Myelofibrosis Associated Non-Cirrhotic Portal Hypertension: A Call to Screening
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- AP
Aditya Patel, DO
Walter Reed National Military Medical Center
silver springs, MD
Presenting Author(s)
Aditya Patel, DO, Zachary Johnston, MD, Dawn Torres, MD
Walter Reed National Military Medical Center, Bethesda, MD
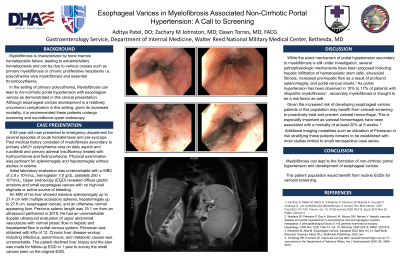
Introduction: Myelofibrosis is characterized by bone marrow hematopoetic failure, leading to extramedullary hematopoiesis and can be secondary to various causes such as primary myelofibrosis or chronic proliferative neoplasms i.e. polycythemia vera myelofibrosis and essential thrombocythemia.1 Mylefibrosis in the setting of primary polycythemia can led to non-cirrhotic portal hypertension with esophageal varices as demonstrated in this clinical presentation. Although esophageal varices are a relatively uncommon complication in this setting given its increased mortality, some have recommended these patients undergo screening and surveillance upper endoscopy.
Case Description/Methods: A 62 year old man presented to emergency department with hematemesis. Past medical history included secondary myelofibrosis from polycythemia vera on daily aspirin and ruxolitinib. Physical examination was pertinent for splenomegaly and hepatomegaly without ascites. Upper endoscopy (EGD) revealed diffuse gastric erosions and small esophageal varices with no high risk stigmata. Initial laboratory evaluation revealed WBC of 2.8 x 103/mcL, hemoglobin 7.0 g/dL, platelets 250 x 103/mcL, and normal liver associated enzymes. An MRI of his liver showed massive splenomegaly up to 27.4 cm, hepatomegaly up to 27.6 cm, esophageal varices, and an otherwise normal appearing liver. He had an unremarkable abdominal doppler ultrasound evaluation with normal hepatic and hepatopetal flow in the portal venous system. Fibroscan was obtained with kPa of 12. Chronic liver disease workup including infectious, autoimmune, and metabolic causes was unremarkable. The patient declined liver biopsy and the plan was made for follow-up EGD in 1 year to survey the small varices seen on the original EGD.
Discussion: While the exact mechanism of portal hypertension secondary to myelofibrosis is still under investigation, several pathophysiologic mechanisms have been proposed including: hepatic infiltration of hematopoietic stem cells, sinusoidal fibrosis, increased pre-hepatic flow as a result of profound splenomegaly, and portal venous insults.2 Portal hypertension has been observed in 10% to 17% of patients with myelofibrosis.3 Given the increased risk of developing esophageal varices, patients in this population may benefit from variceal screening to proactively treat and prevent variceal hemorrhage. The role of fibroscan in risk stratifying these patients remains to be established with most studies limited to small retrospective case series.
Disclosures:
Aditya Patel, DO, Zachary Johnston, MD, Dawn Torres, MD. E0592 - Esophageal Varices in Myelofibrosis Associated Non-Cirrhotic Portal Hypertension: A Call to Screening, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
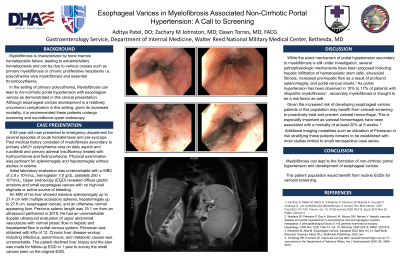
Introduction: Myelofibrosis is characterized by bone marrow hematopoetic failure, leading to extramedullary hematopoiesis and can be secondary to various causes such as primary myelofibrosis or chronic proliferative neoplasms i.e. polycythemia vera myelofibrosis and essential thrombocythemia.1 Mylefibrosis in the setting of primary polycythemia can led to non-cirrhotic portal hypertension with esophageal varices as demonstrated in this clinical presentation. Although esophageal varices are a relatively uncommon complication in this setting given its increased mortality, some have recommended these patients undergo screening and surveillance upper endoscopy.
Case Description/Methods: A 62 year old man presented to emergency department with hematemesis. Past medical history included secondary myelofibrosis from polycythemia vera on daily aspirin and ruxolitinib. Physical examination was pertinent for splenomegaly and hepatomegaly without ascites. Upper endoscopy (EGD) revealed diffuse gastric erosions and small esophageal varices with no high risk stigmata. Initial laboratory evaluation revealed WBC of 2.8 x 103/mcL, hemoglobin 7.0 g/dL, platelets 250 x 103/mcL, and normal liver associated enzymes. An MRI of his liver showed massive splenomegaly up to 27.4 cm, hepatomegaly up to 27.6 cm, esophageal varices, and an otherwise normal appearing liver. He had an unremarkable abdominal doppler ultrasound evaluation with normal hepatic and hepatopetal flow in the portal venous system. Fibroscan was obtained with kPa of 12. Chronic liver disease workup including infectious, autoimmune, and metabolic causes was unremarkable. The patient declined liver biopsy and the plan was made for follow-up EGD in 1 year to survey the small varices seen on the original EGD.
Discussion: While the exact mechanism of portal hypertension secondary to myelofibrosis is still under investigation, several pathophysiologic mechanisms have been proposed including: hepatic infiltration of hematopoietic stem cells, sinusoidal fibrosis, increased pre-hepatic flow as a result of profound splenomegaly, and portal venous insults.2 Portal hypertension has been observed in 10% to 17% of patients with myelofibrosis.3 Given the increased risk of developing esophageal varices, patients in this population may benefit from variceal screening to proactively treat and prevent variceal hemorrhage. The role of fibroscan in risk stratifying these patients remains to be established with most studies limited to small retrospective case series.
Disclosures:
Aditya Patel indicated no relevant financial relationships.
Zachary Johnston indicated no relevant financial relationships.
Dawn Torres indicated no relevant financial relationships.
Aditya Patel, DO, Zachary Johnston, MD, Dawn Torres, MD. E0592 - Esophageal Varices in Myelofibrosis Associated Non-Cirrhotic Portal Hypertension: A Call to Screening, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
