Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0593 - Partial Splenic Artery Embolization for Patients With Portal Hypertension Undergoing Organ Transplant Evaluation: A Case Series
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Lauren Shaffer, MD
University of Pennsylvania
Philadelphia, PA
Presenting Author(s)
Lauren Shaffer, MD, David Kaplan, MD
University of Pennsylvania, Philadelphia, PA
Introduction: Partial splenic artery embolization (PSAE) is an infrequently utilized approach to reduce portal hypertension (PHT) by reducing splenic arterial inflow and thereby splenic vein flow into the portal vein. We describe three patients who underwent PSAE to address diverse manifestations of PHT due to contraindications to transjugular intrahepatic portosystemic shunts (TIPS).
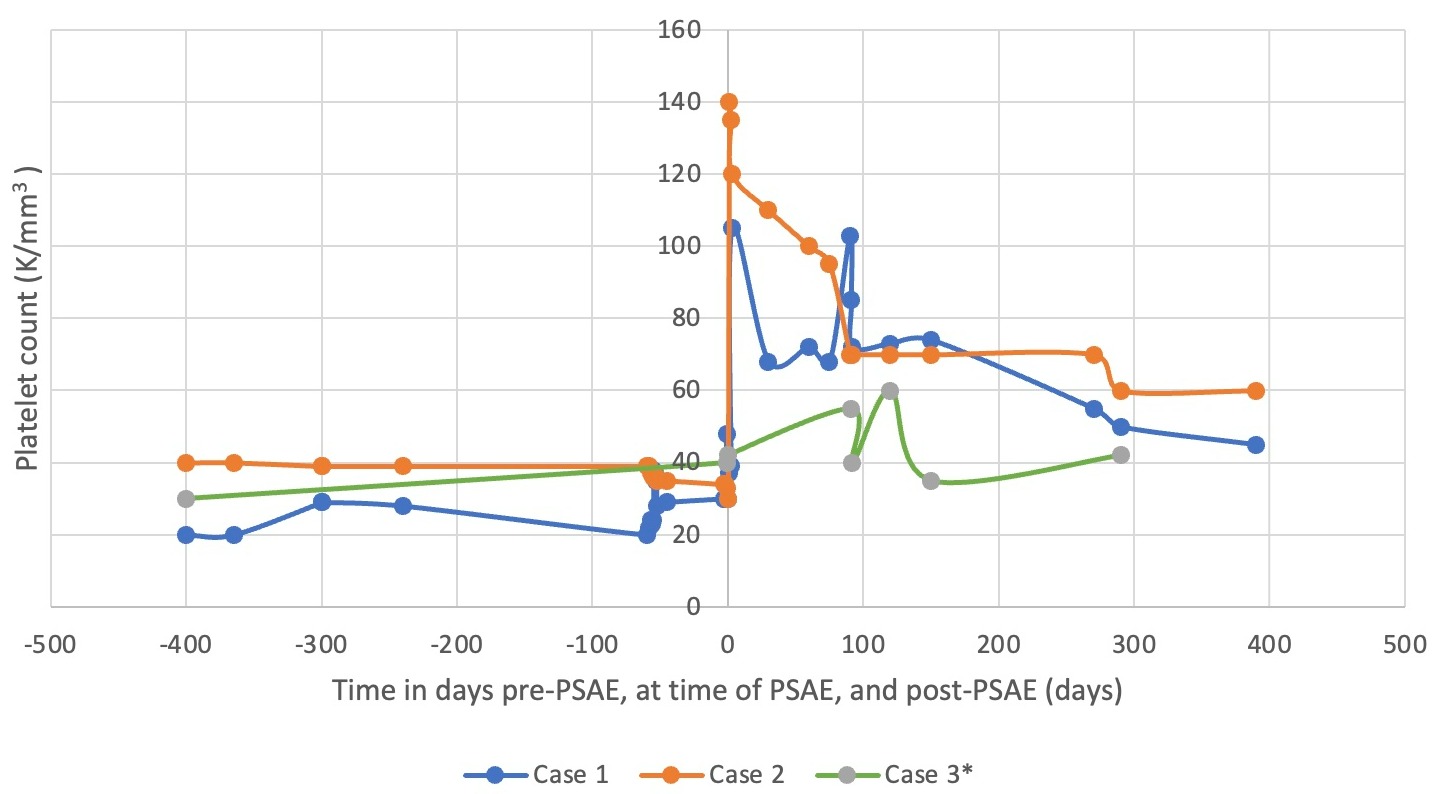
Case Description/Methods: Case 1: A 50-year-old male with CKD stage 4 and idiopathic PHT had diuretic-refractory ascites and thrombocytopenia, precluding surgery for an arteriovenous fistula (AVF) and kidney transplantation. He was not a candidate for TIPS due to extensive portal vein thrombosis but underwent PSAE leading to resolution of ascites and marked improvement in thrombocytopenia (Fig 1). The patient ultimately received an AVF and was placed on the kidney transplant waitlist. He has been followed for 30 months with sustained clinical improvement.
Case 2: A 60-year-old male with prior hepatocellular carcinoma (HCC) status post right partial hepatectomy and hepatitis C cirrhosis complicated by severe thrombocytopenia and refractory ascites, had two previously aborted TIPS procedures due to unusual hepatic vein anatomy. He underwent PSAE that led to a reduction in frequency of therapeutic paracenteses and improvement of thrombocytopenia (Fig 1). Eight months later, TIPS was reattempted and resulted in complete ascites control for over six years. He is currently on the waitlist for liver transplantation.
Case 3: A 60-year-old male had cryptogenic cirrhosis complicated by mild ascites, significant thrombocytopenia, and massive splenomegaly with mass effects. He underwent successful PSAE to alleviate splenic compression of the bladder. One year later, he had a repeat PSAE for diaphragmatic compression secondary to splenic hypertrophy. His thrombocytopenia also mildly improved (Fig 1). The patient was declined for liver transplant due to lack of social support. He expired from advanced HCC after two years of follow-up.
Discussion: We report three cases of PSAE in patients with PHT awaiting organ transplantation. All three cases had improvement in ascites, splenomegaly, and thrombocytopenia. Although PSAE is not the primary treatment for PHT, it may have a therapeutic role in advanced cases, particularly in transplant candidates when other interventions like TIPS are not possible. Future studies should be conducted to further evaluate the role of PSAE in patients with PHT awaiting organ transplantation.
Disclosures:
Lauren Shaffer, MD, David Kaplan, MD. E0593 - Partial Splenic Artery Embolization for Patients With Portal Hypertension Undergoing Organ Transplant Evaluation: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Pennsylvania, Philadelphia, PA
Introduction: Partial splenic artery embolization (PSAE) is an infrequently utilized approach to reduce portal hypertension (PHT) by reducing splenic arterial inflow and thereby splenic vein flow into the portal vein. We describe three patients who underwent PSAE to address diverse manifestations of PHT due to contraindications to transjugular intrahepatic portosystemic shunts (TIPS).
Case Description/Methods: Case 1: A 50-year-old male with CKD stage 4 and idiopathic PHT had diuretic-refractory ascites and thrombocytopenia, precluding surgery for an arteriovenous fistula (AVF) and kidney transplantation. He was not a candidate for TIPS due to extensive portal vein thrombosis but underwent PSAE leading to resolution of ascites and marked improvement in thrombocytopenia (Fig 1). The patient ultimately received an AVF and was placed on the kidney transplant waitlist. He has been followed for 30 months with sustained clinical improvement.
Case 2: A 60-year-old male with prior hepatocellular carcinoma (HCC) status post right partial hepatectomy and hepatitis C cirrhosis complicated by severe thrombocytopenia and refractory ascites, had two previously aborted TIPS procedures due to unusual hepatic vein anatomy. He underwent PSAE that led to a reduction in frequency of therapeutic paracenteses and improvement of thrombocytopenia (Fig 1). Eight months later, TIPS was reattempted and resulted in complete ascites control for over six years. He is currently on the waitlist for liver transplantation.
Case 3: A 60-year-old male had cryptogenic cirrhosis complicated by mild ascites, significant thrombocytopenia, and massive splenomegaly with mass effects. He underwent successful PSAE to alleviate splenic compression of the bladder. One year later, he had a repeat PSAE for diaphragmatic compression secondary to splenic hypertrophy. His thrombocytopenia also mildly improved (Fig 1). The patient was declined for liver transplant due to lack of social support. He expired from advanced HCC after two years of follow-up.
Discussion: We report three cases of PSAE in patients with PHT awaiting organ transplantation. All three cases had improvement in ascites, splenomegaly, and thrombocytopenia. Although PSAE is not the primary treatment for PHT, it may have a therapeutic role in advanced cases, particularly in transplant candidates when other interventions like TIPS are not possible. Future studies should be conducted to further evaluate the role of PSAE in patients with PHT awaiting organ transplantation.
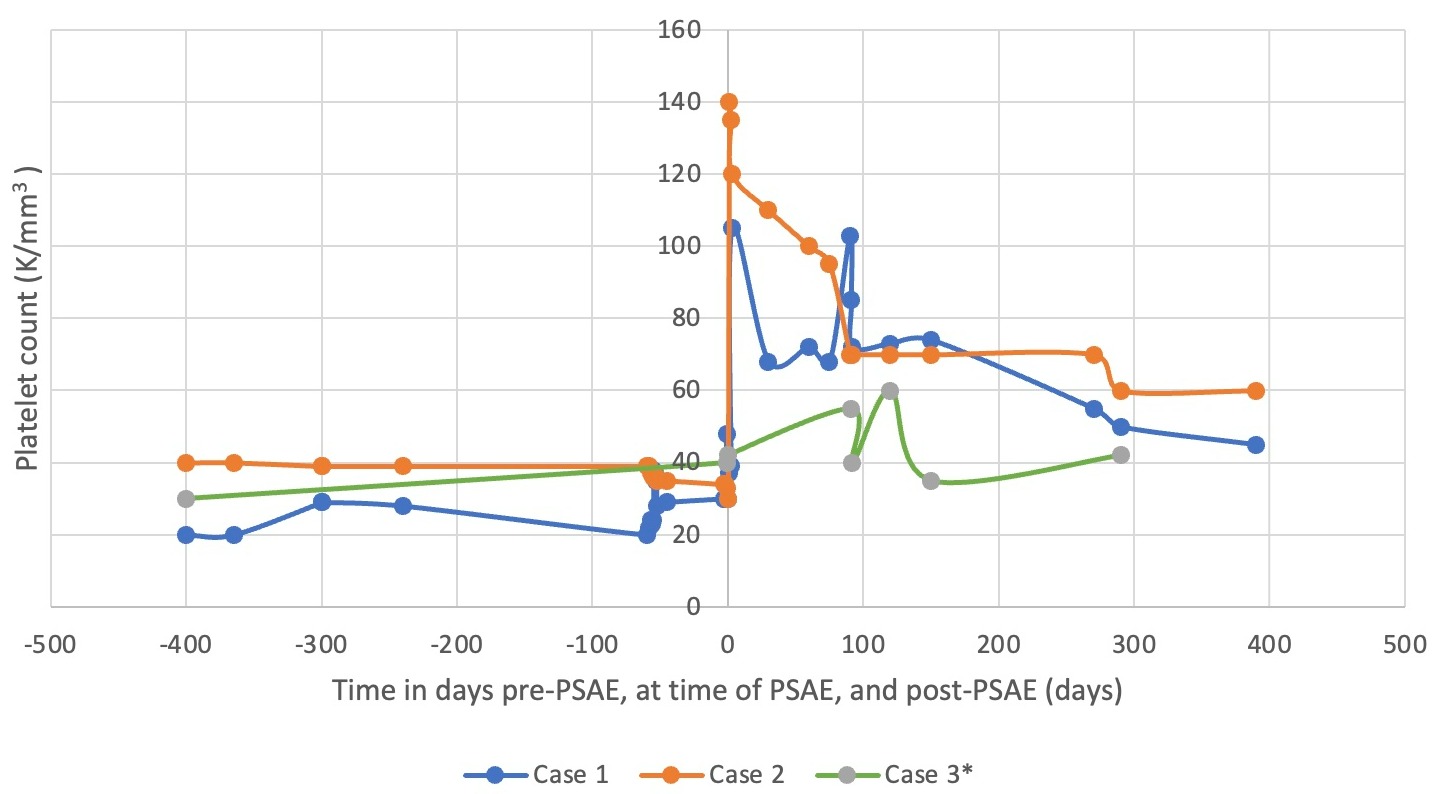
Figure: *2nd PSAE attempt in case 3 represented at time 0
Disclosures:
Lauren Shaffer indicated no relevant financial relationships.
David Kaplan: AstraZeneca Inc – Grant/Research Support. Bayer Healthcare Inc – Grant/Research Support. Exact Sciences Inc. – Grant/Research Support. Gilead Inc. – Grant/Research Support. Glycotest Inc – Grant/Research Support.
Lauren Shaffer, MD, David Kaplan, MD. E0593 - Partial Splenic Artery Embolization for Patients With Portal Hypertension Undergoing Organ Transplant Evaluation: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

