Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0596 - Autoimmune Hepatitis Presenting with Concomitant Chronic Pancreatitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Dhruv Patel, DO
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Ahmed Salem, MD1, Dhruv Patel, DO1, Brooke E. Kania, DO2, Mina Fransawy Alkomos, MD3, William Lewis, BS4
1St. Joseph's University Medical Center, Paterson, NJ; 2Saint Joseph's University Medical Center, Parsippany-Troy Hills, NJ; 3Saint Joseph's University Medical Center, Paterson, NJ; 4St. Josephs University Medical Center, Paterson, NJ
Introduction: Autoimmune Hepatitis (AIH) is a progressive form of chronic hepatitis, with periods of remissions and exacerbations. Diagnosis includes abnormally high levels of immunoglobulins and multiple autoantibodies, with female predominance. Clinical presentation is variable, with a spectrum extending from asymptomatic cases to fulminant liver failure. Presenting symptoms may include abdominal pain, malaise, fatigue, and small joint arthralgia. We present a case of a 36 YO M with PMH of alcohol dependence and acute pancreatitis who was diagnosed with AIH.
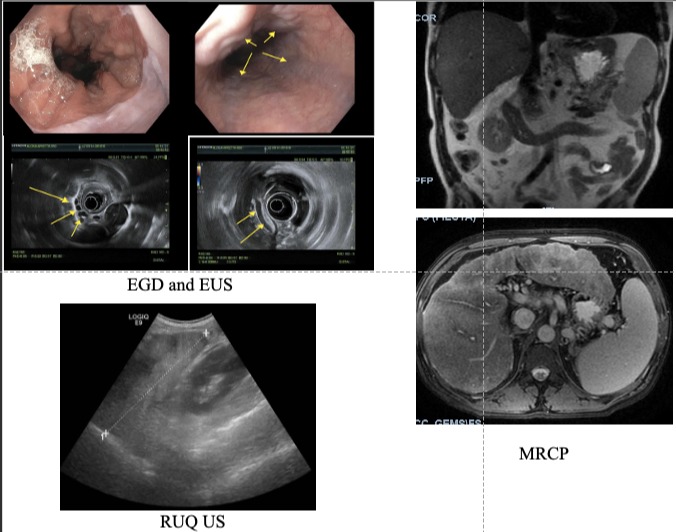
Case Description/Methods: A 36 YO AA M with PMH of alcohol dependence (in remission for 2 yrs), tobacco use, and pancreatitis, presented to the ED with non-radiating mid-epigastric abdominal pain 10/10 in severity, associated with NBNB emesis, exacerbated by movement for 2 days. The patient was hemodynamically stable and on exam he had icteric frenulum, abdominal distension, with liver span 12cm at mid-clavicular line, and absence of fluid wave, shifting dullness, rebound tenderness, or voluntary guarding. Labs notable for pancytopenia, elevated lipase, elevated ALP, elevated AST and ALT with 2:1 ratio, and hyperbilirubinemia. MRCP showed cirrhotic liver with splenomegaly and varices, as well as with free fluid in the lesser sac along the pancreatic head, duodenum, and right retroperitoneum (compatible with acute pancreatitis). Patient received IV fluids for pancreatitis. Additional labs were remarkable for elevated actin smooth muscle antibody at 26U (ref range: 0-19), ANA positive, with high alpha-1-antitrypsin levels and normal ceruloplasmin levels. The patient left against medical advice; and was given resources for Hepatology with referral for liver transplant.
Discussion: There is limited data regarding patients with concomitant AIH and pancreatitis. Our pt presented with a AIH with secondary acute on chronic pancreatitis, in the absence of additional autoimmune manifestations. Mechanism of AIH remains poorly understood; however, there is an association between the HLA gene and AIH. Genetic studies have shown HLA-DRB1*0301 and HLA-DRB1*0401 as primary and secondary genotypes susceptible to AIH, as well as genetic variants with CARD10 and SH2B3. Products secondary to metabolism of ETOH such as alcohol dehydrogenase, malondialdehyde, and acetaldehyde, can lead to development of autoantibodies. Additional research is indicated to evaluate the relationship between AIH and acute pancreatitis.
Disclosures:
Ahmed Salem, MD1, Dhruv Patel, DO1, Brooke E. Kania, DO2, Mina Fransawy Alkomos, MD3, William Lewis, BS4. E0596 - Autoimmune Hepatitis Presenting with Concomitant Chronic Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Saint Joseph's University Medical Center, Parsippany-Troy Hills, NJ; 3Saint Joseph's University Medical Center, Paterson, NJ; 4St. Josephs University Medical Center, Paterson, NJ
Introduction: Autoimmune Hepatitis (AIH) is a progressive form of chronic hepatitis, with periods of remissions and exacerbations. Diagnosis includes abnormally high levels of immunoglobulins and multiple autoantibodies, with female predominance. Clinical presentation is variable, with a spectrum extending from asymptomatic cases to fulminant liver failure. Presenting symptoms may include abdominal pain, malaise, fatigue, and small joint arthralgia. We present a case of a 36 YO M with PMH of alcohol dependence and acute pancreatitis who was diagnosed with AIH.
Case Description/Methods: A 36 YO AA M with PMH of alcohol dependence (in remission for 2 yrs), tobacco use, and pancreatitis, presented to the ED with non-radiating mid-epigastric abdominal pain 10/10 in severity, associated with NBNB emesis, exacerbated by movement for 2 days. The patient was hemodynamically stable and on exam he had icteric frenulum, abdominal distension, with liver span 12cm at mid-clavicular line, and absence of fluid wave, shifting dullness, rebound tenderness, or voluntary guarding. Labs notable for pancytopenia, elevated lipase, elevated ALP, elevated AST and ALT with 2:1 ratio, and hyperbilirubinemia. MRCP showed cirrhotic liver with splenomegaly and varices, as well as with free fluid in the lesser sac along the pancreatic head, duodenum, and right retroperitoneum (compatible with acute pancreatitis). Patient received IV fluids for pancreatitis. Additional labs were remarkable for elevated actin smooth muscle antibody at 26U (ref range: 0-19), ANA positive, with high alpha-1-antitrypsin levels and normal ceruloplasmin levels. The patient left against medical advice; and was given resources for Hepatology with referral for liver transplant.
Discussion: There is limited data regarding patients with concomitant AIH and pancreatitis. Our pt presented with a AIH with secondary acute on chronic pancreatitis, in the absence of additional autoimmune manifestations. Mechanism of AIH remains poorly understood; however, there is an association between the HLA gene and AIH. Genetic studies have shown HLA-DRB1*0301 and HLA-DRB1*0401 as primary and secondary genotypes susceptible to AIH, as well as genetic variants with CARD10 and SH2B3. Products secondary to metabolism of ETOH such as alcohol dehydrogenase, malondialdehyde, and acetaldehyde, can lead to development of autoantibodies. Additional research is indicated to evaluate the relationship between AIH and acute pancreatitis.
Figure: A closer look at the case with images from the EGD, EUS, Right upper quadrant ultrasound and MRCP.
Disclosures:
Ahmed Salem indicated no relevant financial relationships.
Dhruv Patel indicated no relevant financial relationships.
Brooke Kania indicated no relevant financial relationships.
Mina Fransawy Alkomos indicated no relevant financial relationships.
William Lewis indicated no relevant financial relationships.
Ahmed Salem, MD1, Dhruv Patel, DO1, Brooke E. Kania, DO2, Mina Fransawy Alkomos, MD3, William Lewis, BS4. E0596 - Autoimmune Hepatitis Presenting with Concomitant Chronic Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
