Back

Poster Session C - Monday Afternoon
Category: Interventional Endoscopy
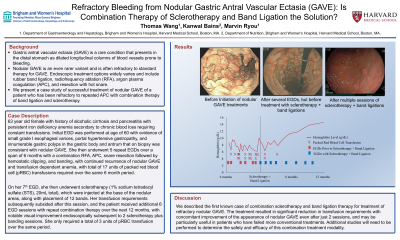
C0470 - Refractory Bleeding From Nodular Gastric Antral Vascular Ectasia (GAVE): Is Combination Therapy of Sclerotherapy and Band Ligation the Solution?
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Thomas Wang, MD
Brigham and Women's Hospital
Boston, MA
Presenting Author(s)
Award: Presidential Poster Award
Thomas Wang, MD1, Kanwal Bains, MBBS2, Marvin Ryou, MD3
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Brigham & Women's Hospital, Boston, MA
Introduction: Gastric antral vascular ectasia (GAVE) is a rare condition that presents in the distal stomach as dilated longitudinal columns of blood vessels prone to bleeding. Nodular GAVE is an even rarer variant and is often refractory to standard therapy for GAVE. Endoscopic treatment options widely varies and include rubber band ligation, radiofrequency ablation (RFA), argon plasma coagulation (APC), and resection with hot snare. We present a case study of successful treatment of nodular GAVE of a patient who has been refractory to repeated APC with combination therapy of band ligation and sclerotherapy.
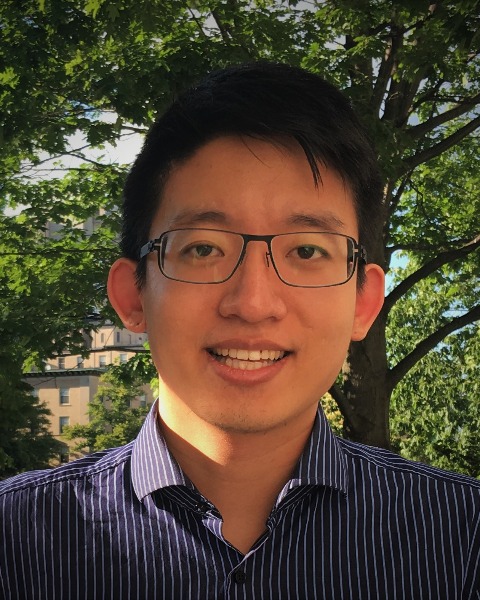
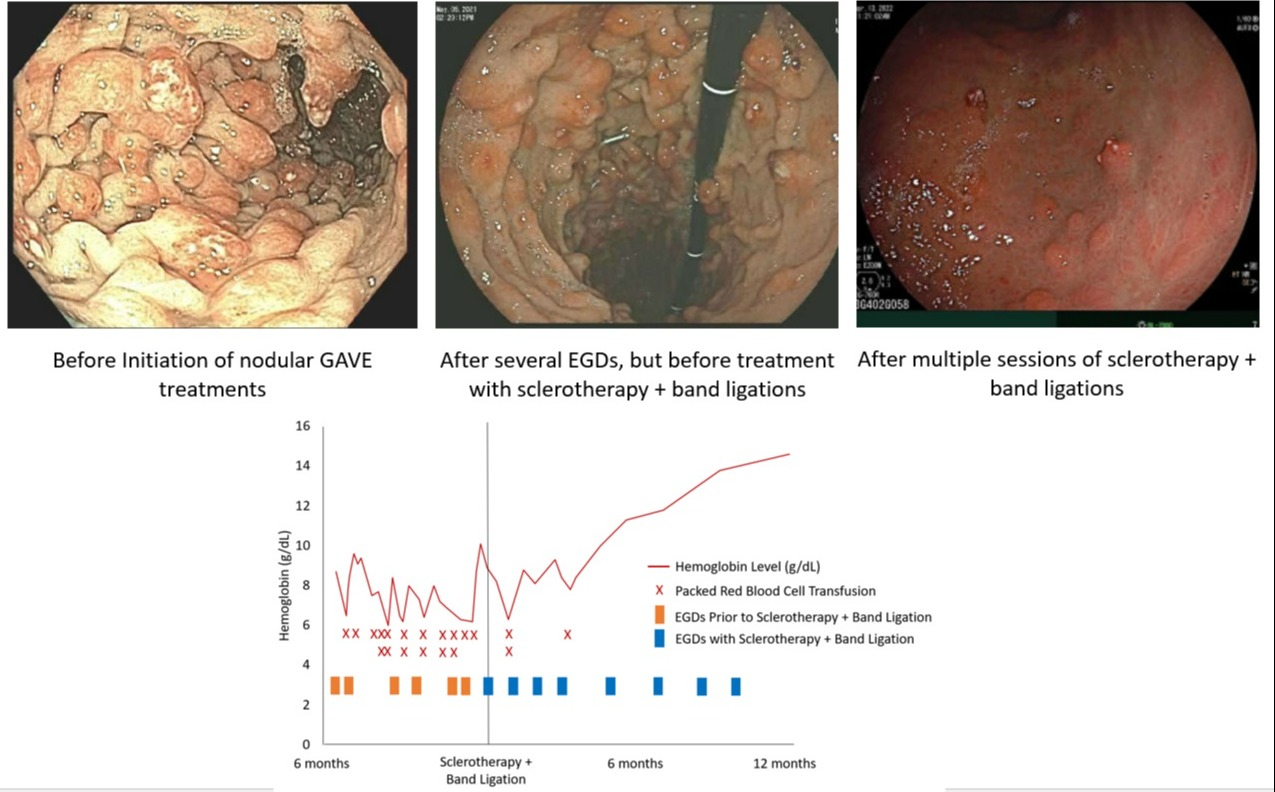
Case Description/Methods: 63 year old female with history of alcoholic cirrhosis and pancreatitis who has had persistent iron deficiency anemia thought secondary to chronic blood loss requiring constant transfusions. Initial EGD was performed at age of 60 with evidence of small grade I esophageal varices, portal hypertensive gastropathy, and innumerable gastric polyps in the gastric body and antrum that on biopsy was consistent with nodular GAVE. She then underwent 5 repeat EGDs over a span of 6 months with a combination RFA, APC, snare resection followed by hemostatic clipping, and banding, with continued recurrence of nodular GAVE and transfusion dependent anemia, with total of 17 units of packed red blood cell (pRBC) transfusions required over the same 6 month period.
On her 7th EGD, she then underwent combination therapy of sclerotherapy (1% sodium tetradecyl sulfate (STS), 20mL total), which were injected at the base of the nodular areas, along with placement of 12 bands. Her transfusion requirements subsequently subsided after the initial sclerotherapy and band ligation combination session, and the patient received additional 6 EGD sessions with repeat combination therapy over the next 12 months, with notable visual improvement endoscopically subsequent to 2 sclerotherapy plus banding sessions. She only required a total of 3 units of pRBC transfusion over the same period.
Discussion: We described the first known case of combination sclerotherapy and band ligation therapy for treatment of refractory nodular GAVE. The treatment resulted in significant reduction in transfusion requirements with concomitant improvement of the appearance of nodular GAVE even after just 2 sessions, and may be particularly useful in patients who have failed more conventional treatments. Additional studies will need to be performed to determine the safety and efficacy of this combination treatment modality.
Disclosures:
Thomas Wang, MD1, Kanwal Bains, MBBS2, Marvin Ryou, MD3. C0470 - Refractory Bleeding From Nodular Gastric Antral Vascular Ectasia (GAVE): Is Combination Therapy of Sclerotherapy and Band Ligation the Solution?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Thomas Wang, MD1, Kanwal Bains, MBBS2, Marvin Ryou, MD3
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Brigham & Women's Hospital, Boston, MA
Introduction: Gastric antral vascular ectasia (GAVE) is a rare condition that presents in the distal stomach as dilated longitudinal columns of blood vessels prone to bleeding. Nodular GAVE is an even rarer variant and is often refractory to standard therapy for GAVE. Endoscopic treatment options widely varies and include rubber band ligation, radiofrequency ablation (RFA), argon plasma coagulation (APC), and resection with hot snare. We present a case study of successful treatment of nodular GAVE of a patient who has been refractory to repeated APC with combination therapy of band ligation and sclerotherapy.
Case Description/Methods: 63 year old female with history of alcoholic cirrhosis and pancreatitis who has had persistent iron deficiency anemia thought secondary to chronic blood loss requiring constant transfusions. Initial EGD was performed at age of 60 with evidence of small grade I esophageal varices, portal hypertensive gastropathy, and innumerable gastric polyps in the gastric body and antrum that on biopsy was consistent with nodular GAVE. She then underwent 5 repeat EGDs over a span of 6 months with a combination RFA, APC, snare resection followed by hemostatic clipping, and banding, with continued recurrence of nodular GAVE and transfusion dependent anemia, with total of 17 units of packed red blood cell (pRBC) transfusions required over the same 6 month period.
On her 7th EGD, she then underwent combination therapy of sclerotherapy (1% sodium tetradecyl sulfate (STS), 20mL total), which were injected at the base of the nodular areas, along with placement of 12 bands. Her transfusion requirements subsequently subsided after the initial sclerotherapy and band ligation combination session, and the patient received additional 6 EGD sessions with repeat combination therapy over the next 12 months, with notable visual improvement endoscopically subsequent to 2 sclerotherapy plus banding sessions. She only required a total of 3 units of pRBC transfusion over the same period.
Discussion: We described the first known case of combination sclerotherapy and band ligation therapy for treatment of refractory nodular GAVE. The treatment resulted in significant reduction in transfusion requirements with concomitant improvement of the appearance of nodular GAVE even after just 2 sessions, and may be particularly useful in patients who have failed more conventional treatments. Additional studies will need to be performed to determine the safety and efficacy of this combination treatment modality.
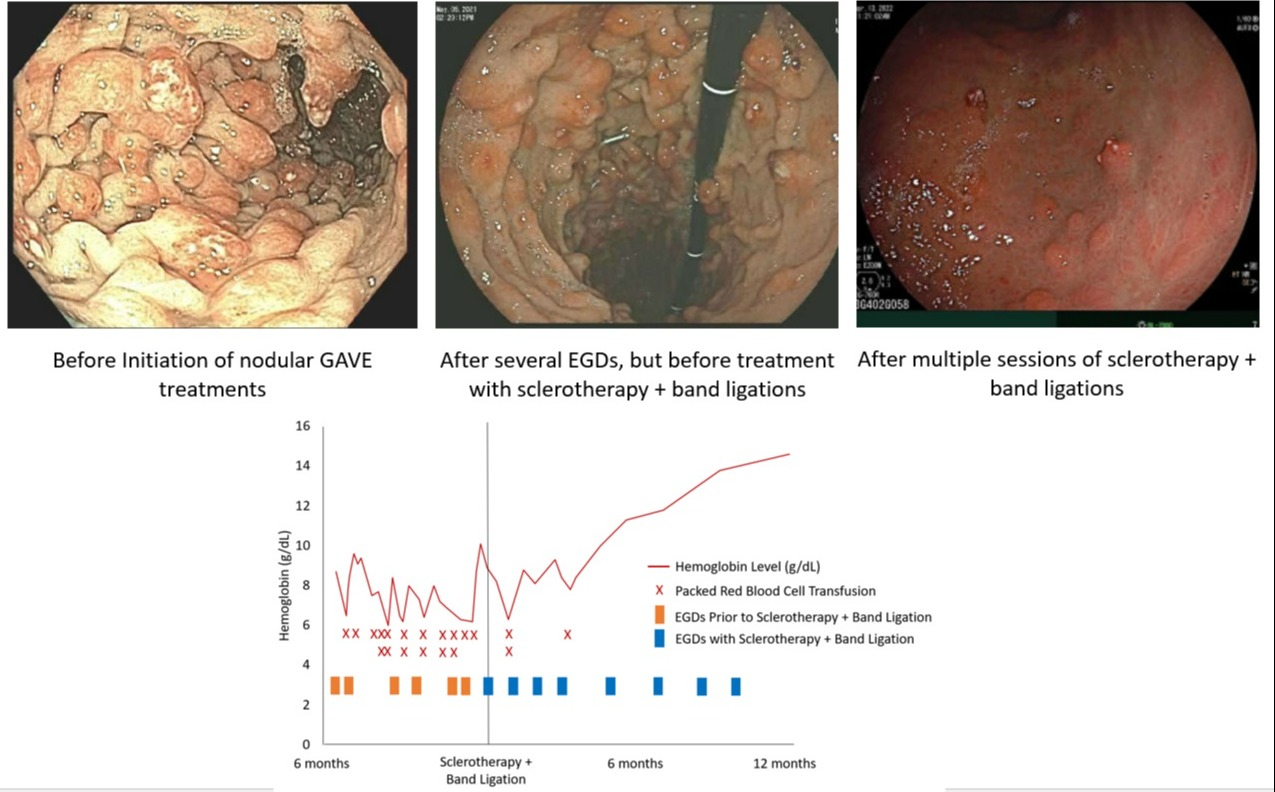
Figure: Figure 1 with endoscopic images of nodular GAVE before and after serial treatments, along with a timeline of hemoglobin level, transfusions, and endoscopic sessions/therapies over the patient's follow up period of 1.5 years
Disclosures:
Thomas Wang indicated no relevant financial relationships.
Kanwal Bains indicated no relevant financial relationships.
Marvin Ryou: Boston Scientific – Consultant. Cook – Consultant. EnteraSense – Consultant, Owner/Ownership Interest. Fuji – Consultant. GI Windows – Consultant, Owner/Ownership Interest. Olympus – Consultant.
Thomas Wang, MD1, Kanwal Bains, MBBS2, Marvin Ryou, MD3. C0470 - Refractory Bleeding From Nodular Gastric Antral Vascular Ectasia (GAVE): Is Combination Therapy of Sclerotherapy and Band Ligation the Solution?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

