Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0603 - Primary Sclerosing Cholangitis Confused for Von Meyenburg Complex
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Dayana Nasr, MD
SUNY Upstate University Hospital
Syracuse, NY
Presenting Author(s)
Dayana Nasr, MD1, Vishnu Kumar, MD2, Pujitha Kudaravalli, MBBS3, Alyssa Ionno, MD3, Janane Nasr, MD4, Ganesh Aswath, MD3
1SUNY Upstate University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3State University of New York Upstate University Hospital, Syracuse, NY; 4Lebanese American University, Beirut, Beyrouth, Lebanon
Introduction: Bile duct hamartomas (BHs), also called von Meyenburg complex (VMC) are benign biliary malformations that are caused by disorganization of the small intrahepatic ducts. Patients are usually symptomatic with jaundice being the most predominant symptom. Abdominal pain and fever are also common. Due to similar findings on CT scan, primary sclerosing cholangitis (PSC) can be mistaken for bile duct hamartomas.
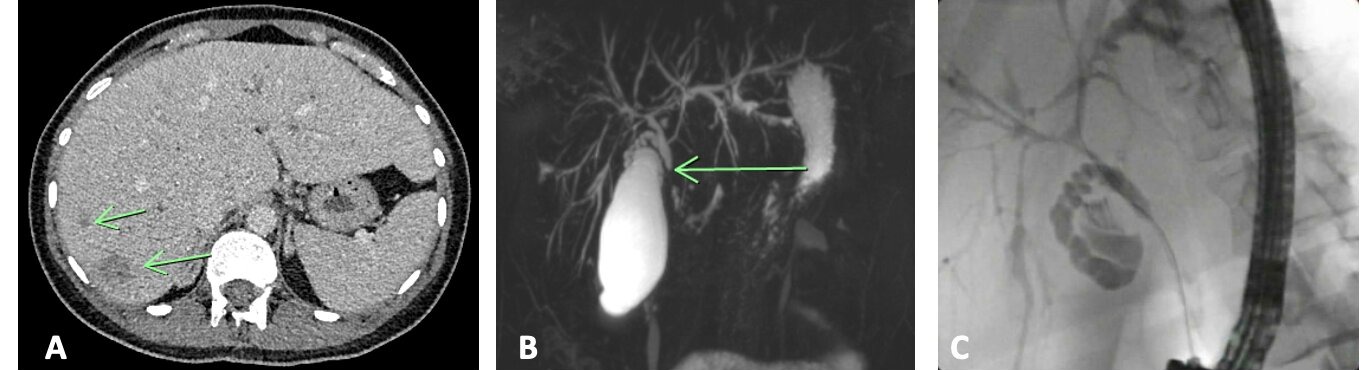
Case Description/Methods: A 30-year-old female presented to the hospital for RUQ abdominal pain, fever, nausea, and vomiting. Liver enzymes were elevated in a cholestatic pattern with ALT of 87 U/L, AST of 71 U/L, ALP of 922 U/L, total bilirubin of 2.1 mg/dl and direct bilirubin of 1.2 mg/dl. CT abdomen with contrast showed numerous nodules suspicious of biliary hamartomas and intrahepatic biliary dilation (Figure 1A). MRI abdomen showed cutoff of the proximal common bile duct (CBD) of unknown etiology but possibly due to stricture, extrinsic compression or intraductal lesion (Figure 1B). ERCP was performed and revealed a single localized biliary stricture in the common hepatic duct in addition to segmental dilation and narrowing of the right and left intrahepatic branches (Figure 1C). No biliary hamartomas were seen. In fact, these findings were highly suggestive of primary sclerosing cholangitis despite negative serology. One plastic stent was placed into the CBD. The patient was later discharged on ursodiol 300 mg 3 times daily. Repeat liver enzymes 2 weeks after discharge showed improvement in liver enzymes and patient continued to deny GI symptoms.
Discussion: The prevalence of BHs varies from 1% in children to 5.6% in adults based on autopsy results while that of PSC is 16.2 cases per 100,000 person-years. They can both present with similar symptoms such as jaundice, abdominal pain, and nausea, although pruritis is also common in PSC. There haven’t been any reported cases where these 2 entities have been confused prior to this one. However, when comparing CT scan findings one can understand why they might be misread. PSC is characterized by a soft-tissue concentric smooth thickening of the extrahepatic biliary duct resulting in mild segmental and often peripheral intrahepatic biliary ducts. Nodules can also be seen as in our case. BHs on plain CT appear as multiple hypodense lesions with irregular and round shape. To achieve the final diagnosis, visualization of the bile ducts by MRCP and ERCP can be performed. In addition, liver biopsies can be obtained to confirm the diagnosis of BHs.
Disclosures:
Dayana Nasr, MD1, Vishnu Kumar, MD2, Pujitha Kudaravalli, MBBS3, Alyssa Ionno, MD3, Janane Nasr, MD4, Ganesh Aswath, MD3. E0603 - Primary Sclerosing Cholangitis Confused for Von Meyenburg Complex, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1SUNY Upstate University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3State University of New York Upstate University Hospital, Syracuse, NY; 4Lebanese American University, Beirut, Beyrouth, Lebanon
Introduction: Bile duct hamartomas (BHs), also called von Meyenburg complex (VMC) are benign biliary malformations that are caused by disorganization of the small intrahepatic ducts. Patients are usually symptomatic with jaundice being the most predominant symptom. Abdominal pain and fever are also common. Due to similar findings on CT scan, primary sclerosing cholangitis (PSC) can be mistaken for bile duct hamartomas.
Case Description/Methods: A 30-year-old female presented to the hospital for RUQ abdominal pain, fever, nausea, and vomiting. Liver enzymes were elevated in a cholestatic pattern with ALT of 87 U/L, AST of 71 U/L, ALP of 922 U/L, total bilirubin of 2.1 mg/dl and direct bilirubin of 1.2 mg/dl. CT abdomen with contrast showed numerous nodules suspicious of biliary hamartomas and intrahepatic biliary dilation (Figure 1A). MRI abdomen showed cutoff of the proximal common bile duct (CBD) of unknown etiology but possibly due to stricture, extrinsic compression or intraductal lesion (Figure 1B). ERCP was performed and revealed a single localized biliary stricture in the common hepatic duct in addition to segmental dilation and narrowing of the right and left intrahepatic branches (Figure 1C). No biliary hamartomas were seen. In fact, these findings were highly suggestive of primary sclerosing cholangitis despite negative serology. One plastic stent was placed into the CBD. The patient was later discharged on ursodiol 300 mg 3 times daily. Repeat liver enzymes 2 weeks after discharge showed improvement in liver enzymes and patient continued to deny GI symptoms.
Discussion: The prevalence of BHs varies from 1% in children to 5.6% in adults based on autopsy results while that of PSC is 16.2 cases per 100,000 person-years. They can both present with similar symptoms such as jaundice, abdominal pain, and nausea, although pruritis is also common in PSC. There haven’t been any reported cases where these 2 entities have been confused prior to this one. However, when comparing CT scan findings one can understand why they might be misread. PSC is characterized by a soft-tissue concentric smooth thickening of the extrahepatic biliary duct resulting in mild segmental and often peripheral intrahepatic biliary ducts. Nodules can also be seen as in our case. BHs on plain CT appear as multiple hypodense lesions with irregular and round shape. To achieve the final diagnosis, visualization of the bile ducts by MRCP and ERCP can be performed. In addition, liver biopsies can be obtained to confirm the diagnosis of BHs.
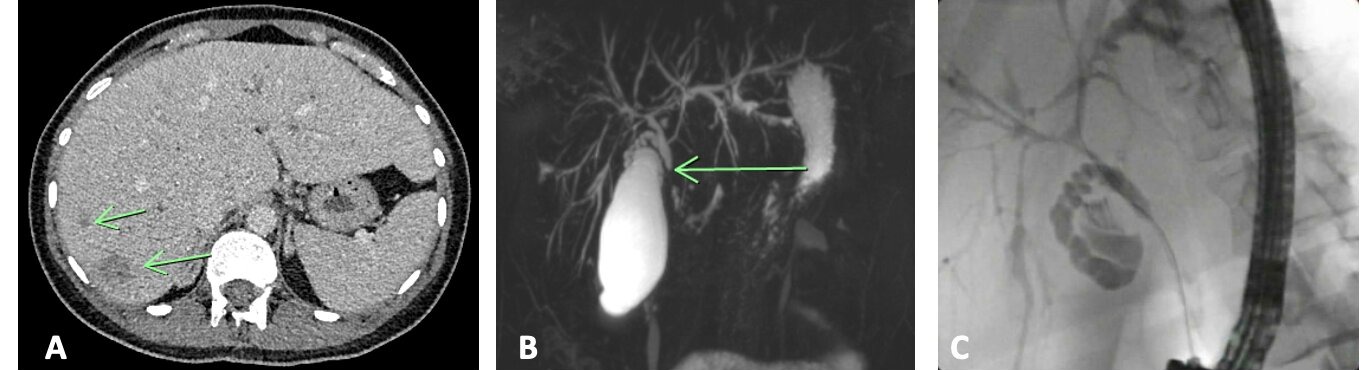
Figure: Figure 1A: Axial CT abdomen of the liver showing multiple non-enhancing hypodense lesions suspicious for hamartomas
Figure 1B: MRCP 3D recon images showing a dilated proximal CBD with distal abrupt loss suggestive of obstruction
Figure 1C: ERCP showing a single localized biliary stricture in the common hepatic duct likely
secondary to primary sclerosing cholangitis
Figure 1B: MRCP 3D recon images showing a dilated proximal CBD with distal abrupt loss suggestive of obstruction
Figure 1C: ERCP showing a single localized biliary stricture in the common hepatic duct likely
secondary to primary sclerosing cholangitis
Disclosures:
Dayana Nasr indicated no relevant financial relationships.
Vishnu Kumar indicated no relevant financial relationships.
Pujitha Kudaravalli indicated no relevant financial relationships.
Alyssa Ionno indicated no relevant financial relationships.
Janane Nasr indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Dayana Nasr, MD1, Vishnu Kumar, MD2, Pujitha Kudaravalli, MBBS3, Alyssa Ionno, MD3, Janane Nasr, MD4, Ganesh Aswath, MD3. E0603 - Primary Sclerosing Cholangitis Confused for Von Meyenburg Complex, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
