Back

Poster Session A - Sunday Afternoon
Category: Liver
A0589 - A Case of Syphilitic Hepatitis (SH): An Elusive Diagnosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- AC
Abhishek A. Chouthai, MD
Cooper Medical School at Rowan University, Cooper University Hospital
New Brunswick, NJ
Presenting Author(s)
Abhishek A. Chouthai, MD1, Alexander Garcia, DO2, Ishita Dhawan, MD2, Christina Capanescu, MD2
1Cooper Medical School at Rowan University, Cooper University Hospital, New Brunswick, NJ; 2Cooper Medical School at Rowan University, Cooper University Hospital, Camden, NJ
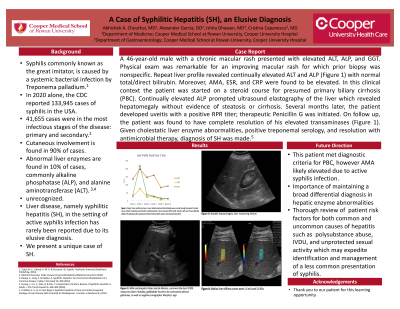
Introduction: Syphilis commonly known as the great imitator, is caused by a systemic bacterial infection by Treponema palladium.1 In 2020 alone, the CDC reported 133,945 cases of syphilis, 41,655 of them from the most infectious stages of the disease: primary and secondary.2 Given its array of clinical manifestations, syphilis can often be difficult to diagnose as reflected by its rising incidence in the US. While clinicians are well adept at identifying the most common clinical, physical exam, and laboratory findings of syphilis infection, some of the rarer abnormalities such as liver involvement can often go unrecognized. While cutaneous involvement of syphilis is found in 90% of cases, abnormal liver enzymes, notably alkaline phosphatase (ALP), is found in 10% of diagnoses.3,4 Liver disease, namely syphilitic hepatitis (SH), in the setting of active syphilis infection has rarely been reported due to its elusive diagnosis. Here we present a unique case of SH.
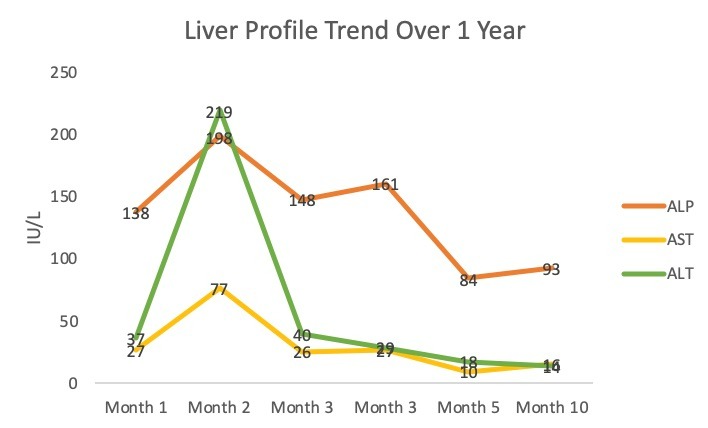
Case Description/Methods: A 46-year-old male with a chronic macular rash presented with elevated ALT, ALP, and GGT. Physical exam was remarkable for an improving macular rash for which prior biopsy was nonspecific. Repeat liver profile revealed continually elevated ALT and ALP (Figure 1) with normal total/direct bilirubin. Moreover, AMA, ESR, and CRP were found to be elevated. In this clinical context the patient was started on a steroid course for presumed primary biliary cirrhosis (PBC). Continually elevated ALP prompted ultrasound elastography of the liver which revealed hepatomegaly without evidence of steatosis or cirrhosis. Several months later, the patient developed uveitis with a positive RPR titer; therapeutic Penicillin G was initiated. On follow up, the patient was found to have complete resolution of his elevated transaminases (Figure 1). Given cholestatic liver enzyme abnormalities, positive treponemal serology, and resolution with antimicrobial therapy, diagnosis of SH was made.5
Discussion: Our case represents the importance of maintaining a broad differential diagnosis in hepatic enzyme abnormalities as well as a review of patient risk factors for both common and uncommon causes of hepatitis. Although patient met diagnostic criteria mimicking PBC, AMA likely was elevated in the setting of active syphilis infection and thereby highlights the importance of reviewing risk factors including polysubstance abuse, IVDU, and unprotected sexual activity which may expedite identification and management of a less common presentation of syphilis.
Disclosures:
Abhishek A. Chouthai, MD1, Alexander Garcia, DO2, Ishita Dhawan, MD2, Christina Capanescu, MD2. A0589 - A Case of Syphilitic Hepatitis (SH): An Elusive Diagnosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cooper Medical School at Rowan University, Cooper University Hospital, New Brunswick, NJ; 2Cooper Medical School at Rowan University, Cooper University Hospital, Camden, NJ
Introduction: Syphilis commonly known as the great imitator, is caused by a systemic bacterial infection by Treponema palladium.1 In 2020 alone, the CDC reported 133,945 cases of syphilis, 41,655 of them from the most infectious stages of the disease: primary and secondary.2 Given its array of clinical manifestations, syphilis can often be difficult to diagnose as reflected by its rising incidence in the US. While clinicians are well adept at identifying the most common clinical, physical exam, and laboratory findings of syphilis infection, some of the rarer abnormalities such as liver involvement can often go unrecognized. While cutaneous involvement of syphilis is found in 90% of cases, abnormal liver enzymes, notably alkaline phosphatase (ALP), is found in 10% of diagnoses.3,4 Liver disease, namely syphilitic hepatitis (SH), in the setting of active syphilis infection has rarely been reported due to its elusive diagnosis. Here we present a unique case of SH.
Case Description/Methods: A 46-year-old male with a chronic macular rash presented with elevated ALT, ALP, and GGT. Physical exam was remarkable for an improving macular rash for which prior biopsy was nonspecific. Repeat liver profile revealed continually elevated ALT and ALP (Figure 1) with normal total/direct bilirubin. Moreover, AMA, ESR, and CRP were found to be elevated. In this clinical context the patient was started on a steroid course for presumed primary biliary cirrhosis (PBC). Continually elevated ALP prompted ultrasound elastography of the liver which revealed hepatomegaly without evidence of steatosis or cirrhosis. Several months later, the patient developed uveitis with a positive RPR titer; therapeutic Penicillin G was initiated. On follow up, the patient was found to have complete resolution of his elevated transaminases (Figure 1). Given cholestatic liver enzyme abnormalities, positive treponemal serology, and resolution with antimicrobial therapy, diagnosis of SH was made.5
Discussion: Our case represents the importance of maintaining a broad differential diagnosis in hepatic enzyme abnormalities as well as a review of patient risk factors for both common and uncommon causes of hepatitis. Although patient met diagnostic criteria mimicking PBC, AMA likely was elevated in the setting of active syphilis infection and thereby highlights the importance of reviewing risk factors including polysubstance abuse, IVDU, and unprotected sexual activity which may expedite identification and management of a less common presentation of syphilis.
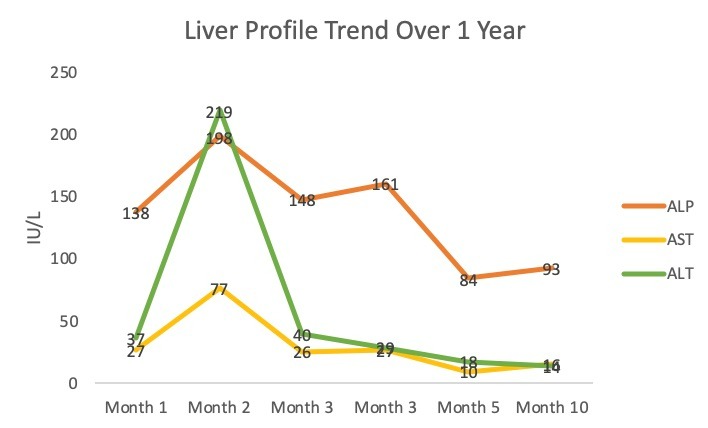
Figure: Patient’s liver profile trend over 1 year. Notably total and direct bilirubin were normal through the patient's clinical course. Month 5 indicates post Penicillin G administration at time of positive RPR (1:256). Patient’s GGT was 279 and AMA 88. [Alkaline Phosphatase (ALP), Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT)]
Disclosures:
Abhishek Chouthai indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Ishita Dhawan indicated no relevant financial relationships.
Christina Capanescu indicated no relevant financial relationships.
Abhishek A. Chouthai, MD1, Alexander Garcia, DO2, Ishita Dhawan, MD2, Christina Capanescu, MD2. A0589 - A Case of Syphilitic Hepatitis (SH): An Elusive Diagnosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
