Back

Poster Session E - Tuesday Afternoon
Category: Small Intestine
E0646 - Bruner’s Gland Hyperplasia Mimicking Duodenal Carcinoma
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Luma Mohsin, MBChB
Christus Spohn Shoreline Hospital
Corpus Christi, TX
Presenting Author(s)
Luma Mohsin, MBChB1, Todd A. Williams, MD2, Bryn Haws, DO3
1Christus Spohn Shoreline Hospital, Corpus Christi, TX; 2Grand Teton Gastroenterology, Idaho Falls, ID; 3Eastern Idaho Regional Medical Center, Idaho Falls, ID
Introduction: Brunner's gland hyperplasia are rare benign tumors, arise from Brunner's glands in the duodenum. Brunner's gland hyperplasia is asymptomatic in many patients but it can present with GI bleed or small bowel obstruction. We are presenting an interesting case of a patient with Brunner's Gland hyperplasia resembling a duodenal carcinoma.
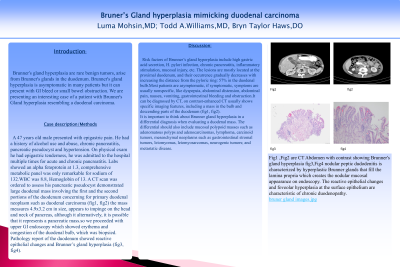
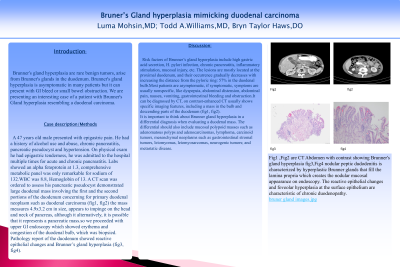
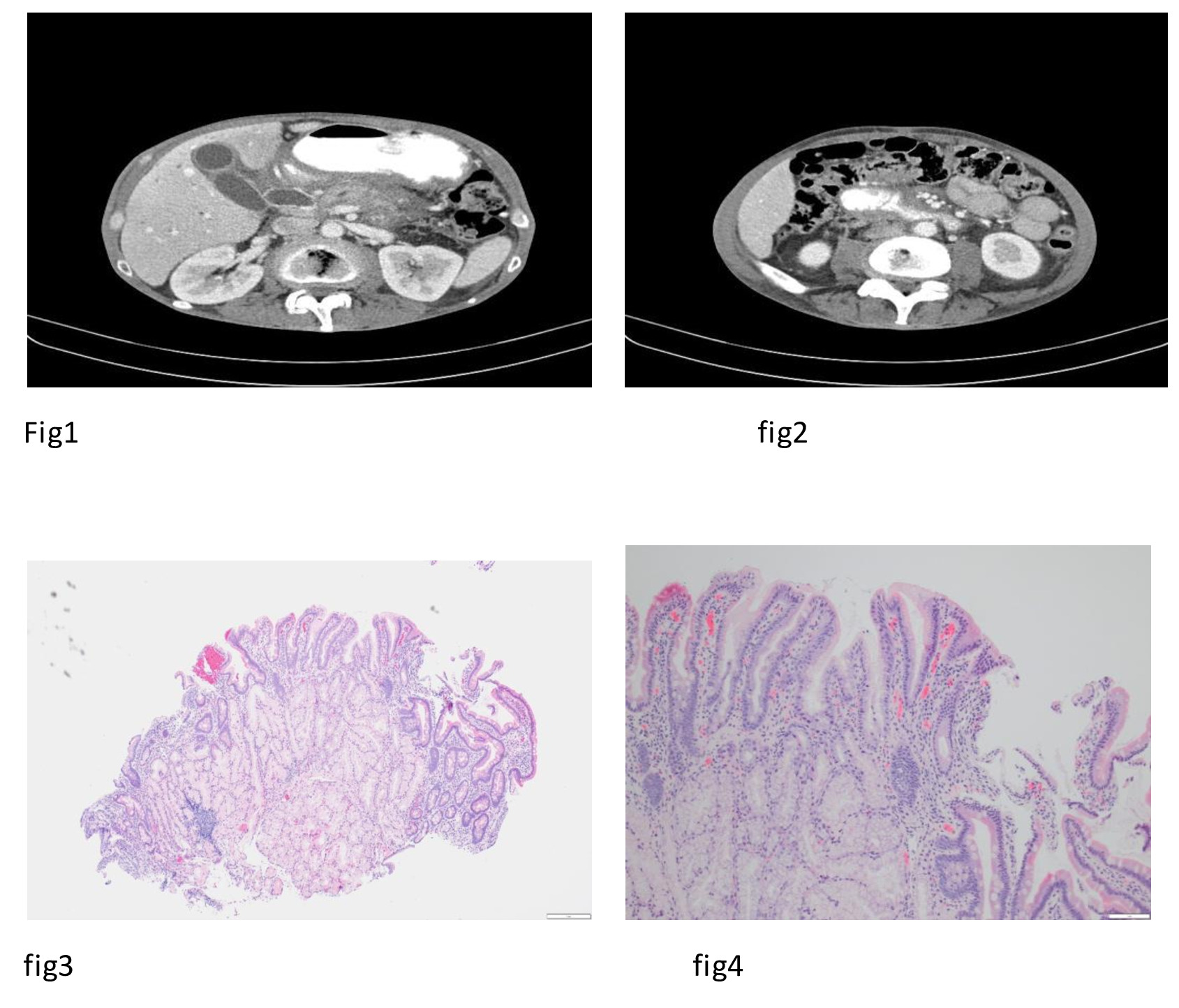
Case Description/Methods: A 47 years old male presented with epigastric pain. He had a history of alcohol use and abuse, chronic pancreatitis, pancreatic pseudocyst and hypertension. On physical exam he had epigastric tenderness, he was admitted to the hospital multiple times for acute and chronic pancreatitis. Labs showed an alpha fetoprotein at 1.3, comprehensive metabolic panel was only remarkable for sodium of 132.WBC was 8.8, Hemoglobin of 13. A CT scan was ordered to assess his pancreatic pseudocyst demonstrated large duodenal mass involving the first and the second portions of the duodenum concerning for primary duodenal neoplasm such as duodenal carcinoma (fig1, fig2) the mass measures 4.9x3.2 cm in size, appears to impinge on the head and neck of pancreas, although it alternatively, it is possible that it represents a pancreatic mass.so we proceeded with upper GI endoscopy which showed erythema and congestion of the duodenal bulb, which was biopsied. Pathology report of the duodenum showed reactive epithelial changes and Brunner’s gland hyperplasia (fig3, fig4).
Discussion: Risk factors of Brunner’s gland hyperplasia include high gastric acid secretion, H. pylori infection, chronic pancreatitis, inflammatory stimulation, mucosal injury, etc. The lesions are mostly located at the proximal duodenum, and their occurrence gradually decreases with increasing the distance from the pyloric ring: 57% in the duodenal bulb.Most patients are asymptomatic, if symptomatic, symptoms are usually nonspecific, like dyspepsia, abdominal distension, abdominal pain, nausea, vomiting, gastrointestinal bleeding and obstruction.It can be diagnosed by CT, on contrast-enhanced CT usually shows specific imaging features, including a mass in the bulb and descending parts of the duodenum (fig1, fig2).
It is important to think about Brunner gland hyperplasia in a differential diagnosis when evaluating a duodenal mass. The differential should also include mucosal polypoid masses such as adenomatous polyps and adenocarcinomas, lymphoma, carcinoid tumors, mesenchymal neoplasms such as gastrointestinal stromal tumors, leiomyomas, leiomyosarcomas, neurogenic tumors; and metastatic disease.
Disclosures:
Luma Mohsin, MBChB1, Todd A. Williams, MD2, Bryn Haws, DO3. E0646 - Bruner’s Gland Hyperplasia Mimicking Duodenal Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Christus Spohn Shoreline Hospital, Corpus Christi, TX; 2Grand Teton Gastroenterology, Idaho Falls, ID; 3Eastern Idaho Regional Medical Center, Idaho Falls, ID
Introduction: Brunner's gland hyperplasia are rare benign tumors, arise from Brunner's glands in the duodenum. Brunner's gland hyperplasia is asymptomatic in many patients but it can present with GI bleed or small bowel obstruction. We are presenting an interesting case of a patient with Brunner's Gland hyperplasia resembling a duodenal carcinoma.
Case Description/Methods: A 47 years old male presented with epigastric pain. He had a history of alcohol use and abuse, chronic pancreatitis, pancreatic pseudocyst and hypertension. On physical exam he had epigastric tenderness, he was admitted to the hospital multiple times for acute and chronic pancreatitis. Labs showed an alpha fetoprotein at 1.3, comprehensive metabolic panel was only remarkable for sodium of 132.WBC was 8.8, Hemoglobin of 13. A CT scan was ordered to assess his pancreatic pseudocyst demonstrated large duodenal mass involving the first and the second portions of the duodenum concerning for primary duodenal neoplasm such as duodenal carcinoma (fig1, fig2) the mass measures 4.9x3.2 cm in size, appears to impinge on the head and neck of pancreas, although it alternatively, it is possible that it represents a pancreatic mass.so we proceeded with upper GI endoscopy which showed erythema and congestion of the duodenal bulb, which was biopsied. Pathology report of the duodenum showed reactive epithelial changes and Brunner’s gland hyperplasia (fig3, fig4).
Discussion: Risk factors of Brunner’s gland hyperplasia include high gastric acid secretion, H. pylori infection, chronic pancreatitis, inflammatory stimulation, mucosal injury, etc. The lesions are mostly located at the proximal duodenum, and their occurrence gradually decreases with increasing the distance from the pyloric ring: 57% in the duodenal bulb.Most patients are asymptomatic, if symptomatic, symptoms are usually nonspecific, like dyspepsia, abdominal distension, abdominal pain, nausea, vomiting, gastrointestinal bleeding and obstruction.It can be diagnosed by CT, on contrast-enhanced CT usually shows specific imaging features, including a mass in the bulb and descending parts of the duodenum (fig1, fig2).
It is important to think about Brunner gland hyperplasia in a differential diagnosis when evaluating a duodenal mass. The differential should also include mucosal polypoid masses such as adenomatous polyps and adenocarcinomas, lymphoma, carcinoid tumors, mesenchymal neoplasms such as gastrointestinal stromal tumors, leiomyomas, leiomyosarcomas, neurogenic tumors; and metastatic disease.
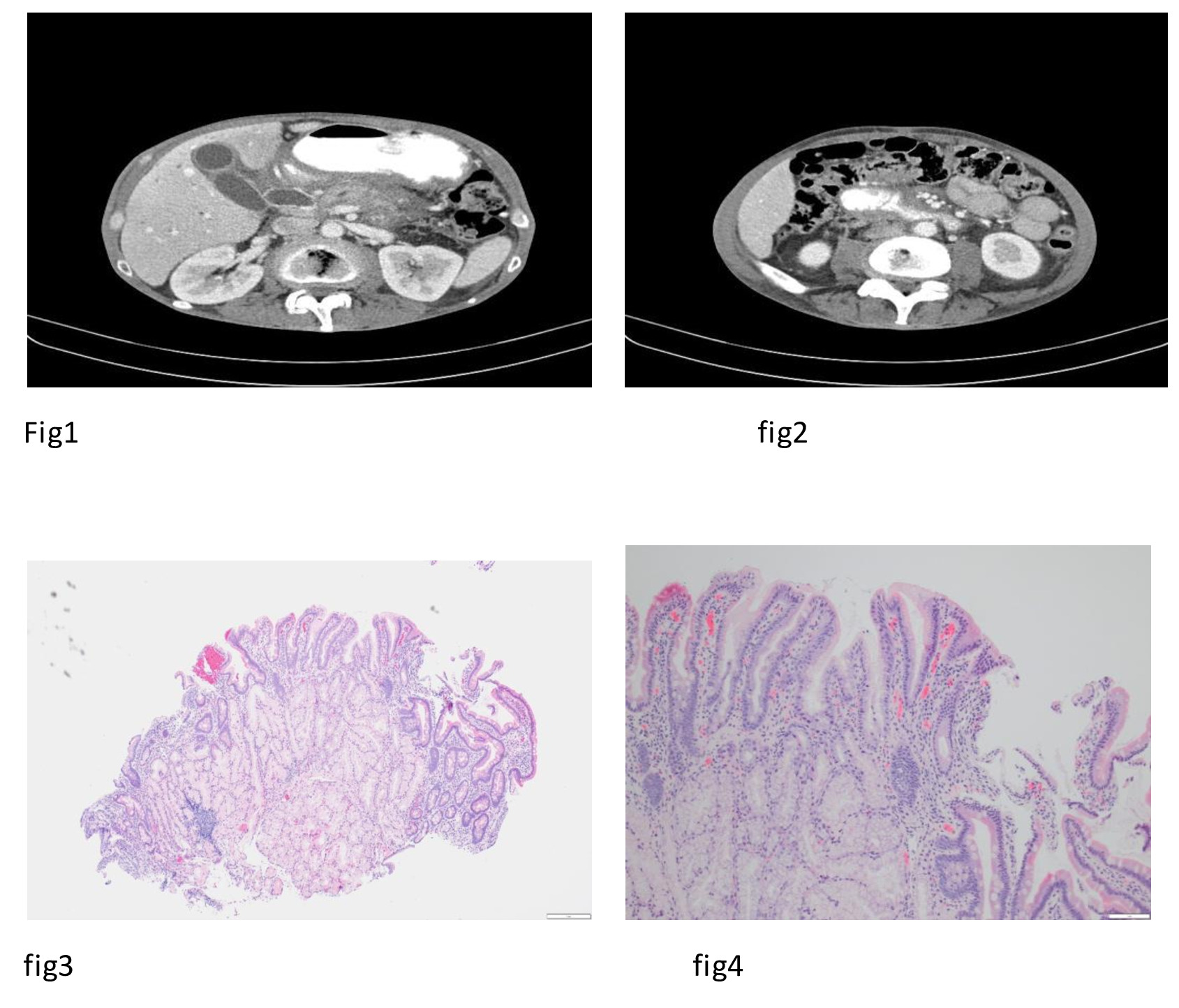
Figure: Fig1 ,Fig2 are CT Abdomen with contrast showing Brunner's gland hyperplasia
fig3,Fig4 nodular peptic dudodenitis is characterized by hyperplastic Brunner glands that fill the lamina propria which creates the nodular mucosal appearance on endoscopy. The reactive epithelial changes and foveolar hyperplasia at the surface epithelium are characteristic of chronic duodenopathy.
fig3,Fig4 nodular peptic dudodenitis is characterized by hyperplastic Brunner glands that fill the lamina propria which creates the nodular mucosal appearance on endoscopy. The reactive epithelial changes and foveolar hyperplasia at the surface epithelium are characteristic of chronic duodenopathy.
Disclosures:
Luma Mohsin indicated no relevant financial relationships.
Todd A. Williams indicated no relevant financial relationships.
Bryn Haws indicated no relevant financial relationships.
Luma Mohsin, MBChB1, Todd A. Williams, MD2, Bryn Haws, DO3. E0646 - Bruner’s Gland Hyperplasia Mimicking Duodenal Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
