Back

Poster Session E - Tuesday Afternoon
Category: Small Intestine
E0673 - A Small Bowel Stricture Revealing Intestinal Lymphoma: A Rare Presentation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sharon Slomovich, MD
Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai
Oceanside, NY
Presenting Author(s)
Sharon Slomovich, MD1, Frank Gress, MD, MBA, FACG2, Ari Steiner, MD3
1Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY; 2Mount Sinai Hospital South Nassau and Icahn School of Medicine at Mount Sinai, Bellmore, NY; 3Mount Sinai South Nassau, Oceanside, NY
Introduction: Lymphoma originating from the gastrointestinal tract is rare. Presenting symptoms are vague and even with the use of advanced imaging and endoscopic techniques, diagnosis is challenging.
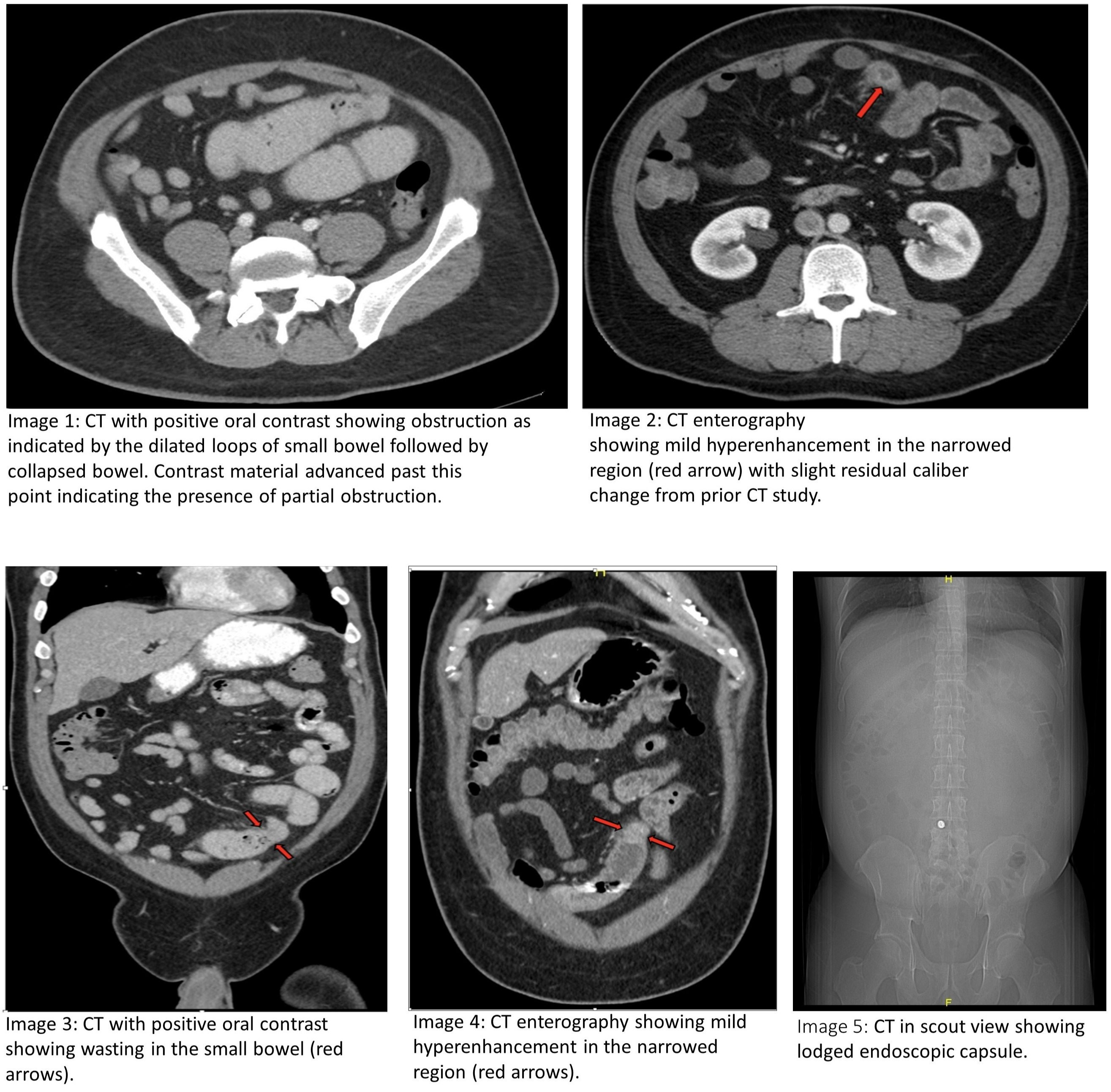
Case Description/Methods: A 43-year-old male with a history of gastroesophageal reflux disease, sarcoidosis (in remission), and hypertension presented with three months of worsening periumbilical pain, a 30-pound weight loss, and repeated emesis. Prior outpatient workup including inflammatory bowel disease (IBD) serology, esophagogastroduodenoscopy, and colonoscopy were unrevealing. Video capsule endoscopy (VCE) demonstrated localized inflammation in the ileum. The capsule was unable to pass beyond this point. On presentation, physical exam was notable for tenderness in the periumbilical area. Routine labs and chest radiograph were normal. CT abdomen/pelvis revealed a partial small bowel obstruction (images 1 and 3). Small bowel enteroscopy (SBE) demonstrated congested mucosa in the proximal ileum, jejunal inflammation, erythematous duodenopathy, and gastritis. Biopsies showed nonspecific chronic inflammation of the ileum and jejunum. CT enterography (CTE) disclosed the presence of a stricture in the mid-ileum (images 2 and 4). The capsule was still seen lodged at the stricture (image 5) but later passed without intervention. ACE levels, calprotectin, and CEA were normal. Stool ova, parasites, and culture for enteric bacteria were negative. Small bowel resection with side-to-side anastomosis was performed. Pathology revealed diffuse large B-cell lymphoma of the small bowel and the patient was started on chemotherapy.
Discussion: A small bowel stricture is rarely attributed to lymphoma and often raises suspicion of an inflammatory process. The stricture in this case was initially thought to be inflammatory given the lack of a bulky mass or lymphadenopathy and evidence of chronic inflammation on biopsies. However, the inflammatory workup for IBD was negative and sarcoidosis was stable, thus further evaluation was required. VCE, SBE with biopsies, and CTE have improved the evaluation of small intestinal pathologies but were nondiagnostic in this case. Due to the patient’s worsening clinical condition and lack of etiology of pathology, more invasive exploration and surgical intervention were warranted and provided the definitive diagnosis. While imaging and endoscopy are crucial in the workup of primary intestinal lymphoma, lack of findings does not rule it out and persistent evaluation is necessary.
Disclosures:
Sharon Slomovich, MD1, Frank Gress, MD, MBA, FACG2, Ari Steiner, MD3. E0673 - A Small Bowel Stricture Revealing Intestinal Lymphoma: A Rare Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY; 2Mount Sinai Hospital South Nassau and Icahn School of Medicine at Mount Sinai, Bellmore, NY; 3Mount Sinai South Nassau, Oceanside, NY
Introduction: Lymphoma originating from the gastrointestinal tract is rare. Presenting symptoms are vague and even with the use of advanced imaging and endoscopic techniques, diagnosis is challenging.
Case Description/Methods: A 43-year-old male with a history of gastroesophageal reflux disease, sarcoidosis (in remission), and hypertension presented with three months of worsening periumbilical pain, a 30-pound weight loss, and repeated emesis. Prior outpatient workup including inflammatory bowel disease (IBD) serology, esophagogastroduodenoscopy, and colonoscopy were unrevealing. Video capsule endoscopy (VCE) demonstrated localized inflammation in the ileum. The capsule was unable to pass beyond this point. On presentation, physical exam was notable for tenderness in the periumbilical area. Routine labs and chest radiograph were normal. CT abdomen/pelvis revealed a partial small bowel obstruction (images 1 and 3). Small bowel enteroscopy (SBE) demonstrated congested mucosa in the proximal ileum, jejunal inflammation, erythematous duodenopathy, and gastritis. Biopsies showed nonspecific chronic inflammation of the ileum and jejunum. CT enterography (CTE) disclosed the presence of a stricture in the mid-ileum (images 2 and 4). The capsule was still seen lodged at the stricture (image 5) but later passed without intervention. ACE levels, calprotectin, and CEA were normal. Stool ova, parasites, and culture for enteric bacteria were negative. Small bowel resection with side-to-side anastomosis was performed. Pathology revealed diffuse large B-cell lymphoma of the small bowel and the patient was started on chemotherapy.
Discussion: A small bowel stricture is rarely attributed to lymphoma and often raises suspicion of an inflammatory process. The stricture in this case was initially thought to be inflammatory given the lack of a bulky mass or lymphadenopathy and evidence of chronic inflammation on biopsies. However, the inflammatory workup for IBD was negative and sarcoidosis was stable, thus further evaluation was required. VCE, SBE with biopsies, and CTE have improved the evaluation of small intestinal pathologies but were nondiagnostic in this case. Due to the patient’s worsening clinical condition and lack of etiology of pathology, more invasive exploration and surgical intervention were warranted and provided the definitive diagnosis. While imaging and endoscopy are crucial in the workup of primary intestinal lymphoma, lack of findings does not rule it out and persistent evaluation is necessary.
Figure: CT abdomen and pelvis with partial small bowel obstruction and CT enterography showing a stricture in the mid-ileum.
Disclosures:
Sharon Slomovich indicated no relevant financial relationships.
Frank Gress indicated no relevant financial relationships.
Ari Steiner indicated no relevant financial relationships.
Sharon Slomovich, MD1, Frank Gress, MD, MBA, FACG2, Ari Steiner, MD3. E0673 - A Small Bowel Stricture Revealing Intestinal Lymphoma: A Rare Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
