Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0416 - Ischemic Colitis Imitating Inflammatory Bowel Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Hiral Patel, MD
Internal Medicine Residency Program, Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Hiral Patel, MD1, Scott Thiesfeldt, MD2, Willie Moore, MD3
1Internal Medicine Residency Program, Wake Forest University School of Medicine, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Inflammatory bowel disease (IBD) and ischemic colitis (IC) are two different entities that can present similarly. There have been case reports of Crohn’s disease mimicking IC in elderly population. In contrast, we present a case of a young patient whose clinical history was consistent with IBD, but he was ultimately found to have IC on biopsy results.
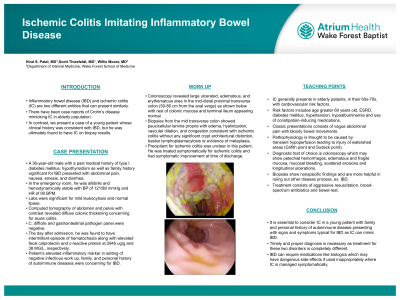
Case Description/Methods: A 36-year-old male with a history of type I diabetes mellitus, hypothyroidism as well as family history significant for IBD presented with abdominal pain, nausea, emesis, and diarrhea. In the emergency room, he was afebrile and hemodynamically stable with BP of 121/88 mmHg and HR of 90 BPM. Labs were significant for mild leukocytosis and normal lipase. Computed tomography of abdomen pelvis with contrast revealed diffuse colonic thickening concerning for acute colitis. C. difficile and gastrointestinal pathogen panel were negative. The day after admission, he was found to have intermittent episode of hematochezia along with elevated fecal calprotectin and c-reactive protein at 2945 ug/g and 38 MG/L respectively. Patient’s elevated inflammatory marker in setting of negative infectious work up, family, and personal history of autoimmune diseases were concerning for IBD. Patient underwent colonoscopy which revealed large ulcerated, edematous, and erythematous area in the mid-distal proximal transverse colon (50-80cm from the anal verge) (Figure 1) with rest of colonic mucosa and terminal ileum appearing normal. Biopsies from the mid transverse colon showed paucicellular lamina propria with edema, hyalinization, vascular dilation, and congestion consistent with ischemic colitis without any significant crypt architectural distortion, basilar lymphoplasmacytosis or evidence of metaplasia. Precipitant for ischemic colitis was unclear in this patient. He was treated symptomatically for ischemic colitis and had symptomatic improvement at time of discharge.
Discussion:
It is essential to consider IC in a young patient with family and personal history of autoimmune disease presenting with signs and symptoms typical for IBD as IC can mimic IBD. Timely and proper diagnosis is necessary as treatment for these two disorders is completely different. IBD can require medications like biologics which may have dangerous side effects if used inappropriately where IC is managed symptomatically.

Disclosures:
Hiral Patel, MD1, Scott Thiesfeldt, MD2, Willie Moore, MD3. E0416 - Ischemic Colitis Imitating Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Internal Medicine Residency Program, Wake Forest University School of Medicine, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Inflammatory bowel disease (IBD) and ischemic colitis (IC) are two different entities that can present similarly. There have been case reports of Crohn’s disease mimicking IC in elderly population. In contrast, we present a case of a young patient whose clinical history was consistent with IBD, but he was ultimately found to have IC on biopsy results.
Case Description/Methods: A 36-year-old male with a history of type I diabetes mellitus, hypothyroidism as well as family history significant for IBD presented with abdominal pain, nausea, emesis, and diarrhea. In the emergency room, he was afebrile and hemodynamically stable with BP of 121/88 mmHg and HR of 90 BPM. Labs were significant for mild leukocytosis and normal lipase. Computed tomography of abdomen pelvis with contrast revealed diffuse colonic thickening concerning for acute colitis. C. difficile and gastrointestinal pathogen panel were negative. The day after admission, he was found to have intermittent episode of hematochezia along with elevated fecal calprotectin and c-reactive protein at 2945 ug/g and 38 MG/L respectively. Patient’s elevated inflammatory marker in setting of negative infectious work up, family, and personal history of autoimmune diseases were concerning for IBD. Patient underwent colonoscopy which revealed large ulcerated, edematous, and erythematous area in the mid-distal proximal transverse colon (50-80cm from the anal verge) (Figure 1) with rest of colonic mucosa and terminal ileum appearing normal. Biopsies from the mid transverse colon showed paucicellular lamina propria with edema, hyalinization, vascular dilation, and congestion consistent with ischemic colitis without any significant crypt architectural distortion, basilar lymphoplasmacytosis or evidence of metaplasia. Precipitant for ischemic colitis was unclear in this patient. He was treated symptomatically for ischemic colitis and had symptomatic improvement at time of discharge.
Discussion:
It is essential to consider IC in a young patient with family and personal history of autoimmune disease presenting with signs and symptoms typical for IBD as IC can mimic IBD. Timely and proper diagnosis is necessary as treatment for these two disorders is completely different. IBD can require medications like biologics which may have dangerous side effects if used inappropriately where IC is managed symptomatically.

Figure: Colonoscopy showing large edematous and erythematous area in the mid-distal proximal transverse colon
Disclosures:
Hiral Patel indicated no relevant financial relationships.
Scott Thiesfeldt indicated no relevant financial relationships.
Willie Moore indicated no relevant financial relationships.
Hiral Patel, MD1, Scott Thiesfeldt, MD2, Willie Moore, MD3. E0416 - Ischemic Colitis Imitating Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
