Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0424 - Poor Bowel Preparation or Ileosigmoid Fistula: An Interesting Complication of Fistulizing Crohn’s Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Jeremy Polman, DO, MS, MBA
Baton Rouge General Medical Center
Baton Rouge, LA
Presenting Author(s)
Jeremy Polman, DO, MS, MBA1, Gabrielle Sanford, MD2, J Casey Chapman, MD3, Randee Kidder, FNP4
1Baton Rouge General Medical Center, Baton Rouge, LA; 2LSUHSC Baton Rouge Internal Medicine Residency Program at Our Lady of the Lake, Baton Rouge, LA; 3GI Alliance; Crohn's and Colitis Center at the Baton Rouge General; Louisiana State University Health Sciences Center, Baton Rouge, LA; 4Crohn’s & Colitis Center at the Baton Rouge General, Baton Rouge, LA
Introduction: Fistulas are a relatively common complication of severe Crohn’s disease (CD), which affects up to 50% of patients. Fistula formation is believed to be secondary to bowel inflammation, leading to defects in the epithelial barrier. These defects can lead to penetration and breakdown of neighboring tissues, leading to the formation of a fistula. Fistulas are classically named relative to their anatomic location. Here, the authors present a patient with an interestingly located fistula, preventing successful bowel preparation for colonoscopy.
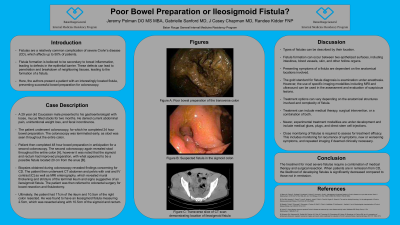
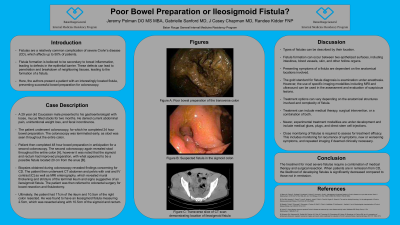
Case Description/Methods: A 29 year old Caucasian male presented to his gastroenterologist with loose stools for two months. He described occasionally noticing mucus in his bowel movements. He denied current abdominal pain, unintentional weight loss, and fecal incontinence. He also denied family history and previous diagnosis of inflammatory bowel disease. The patient underwent colonoscopy, for which he completed 24 hour bowel preparation. The colonoscopy was terminated early, as stool was seen throughout the entire colon. Patient then completed 48 hour bowel preparation in anticipation for a second colonoscopy. The second colonoscopy again revealed stool throughout the entire colon [A], however it was noted that the sigmoid and rectum had improved preparation, with what appeared to be a possible fistula located 20 cm from the anus [B, C]. Yellow liquid output was noted from the possible fistula. Biopsies obtained during colonoscopy revealed findings concerning for CD. The patient then underwent CT abdomen and pelvis with oral and IV contrast as well as MRI enterography, which revealed mural thickening and stricture of the terminal ileum and signs suggestive of an ileosigmoid fistula. The patient was then referred to colorectal surgery for bowel resection and fistulectomy. Ultimately, the patient had 17cm of the ileum and 10.5cm of the right colon resected. He was found to have an ileosigmoid fistula measuring 2.5cm, which was resected along with 10.5cm of the sigmoid and rectum. Postoperatively, patient was referred to an IBD comprehensive care center, where biologic therapy with infliximab was initiated. Patient has had complete resolution of his presenting symptoms and continues to tolerate therapy without complications.
Discussion: The treatment for most fistulas require surgical resection along with medical therapy. When patients are in remission from CD, the likelihood of developing fistulas is significantly decreased compared to those not in remission.

Disclosures:
Jeremy Polman, DO, MS, MBA1, Gabrielle Sanford, MD2, J Casey Chapman, MD3, Randee Kidder, FNP4. E0424 - Poor Bowel Preparation or Ileosigmoid Fistula: An Interesting Complication of Fistulizing Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Baton Rouge General Medical Center, Baton Rouge, LA; 2LSUHSC Baton Rouge Internal Medicine Residency Program at Our Lady of the Lake, Baton Rouge, LA; 3GI Alliance; Crohn's and Colitis Center at the Baton Rouge General; Louisiana State University Health Sciences Center, Baton Rouge, LA; 4Crohn’s & Colitis Center at the Baton Rouge General, Baton Rouge, LA
Introduction: Fistulas are a relatively common complication of severe Crohn’s disease (CD), which affects up to 50% of patients. Fistula formation is believed to be secondary to bowel inflammation, leading to defects in the epithelial barrier. These defects can lead to penetration and breakdown of neighboring tissues, leading to the formation of a fistula. Fistulas are classically named relative to their anatomic location. Here, the authors present a patient with an interestingly located fistula, preventing successful bowel preparation for colonoscopy.
Case Description/Methods: A 29 year old Caucasian male presented to his gastroenterologist with loose stools for two months. He described occasionally noticing mucus in his bowel movements. He denied current abdominal pain, unintentional weight loss, and fecal incontinence. He also denied family history and previous diagnosis of inflammatory bowel disease. The patient underwent colonoscopy, for which he completed 24 hour bowel preparation. The colonoscopy was terminated early, as stool was seen throughout the entire colon. Patient then completed 48 hour bowel preparation in anticipation for a second colonoscopy. The second colonoscopy again revealed stool throughout the entire colon [A], however it was noted that the sigmoid and rectum had improved preparation, with what appeared to be a possible fistula located 20 cm from the anus [B, C]. Yellow liquid output was noted from the possible fistula. Biopsies obtained during colonoscopy revealed findings concerning for CD. The patient then underwent CT abdomen and pelvis with oral and IV contrast as well as MRI enterography, which revealed mural thickening and stricture of the terminal ileum and signs suggestive of an ileosigmoid fistula. The patient was then referred to colorectal surgery for bowel resection and fistulectomy. Ultimately, the patient had 17cm of the ileum and 10.5cm of the right colon resected. He was found to have an ileosigmoid fistula measuring 2.5cm, which was resected along with 10.5cm of the sigmoid and rectum. Postoperatively, patient was referred to an IBD comprehensive care center, where biologic therapy with infliximab was initiated. Patient has had complete resolution of his presenting symptoms and continues to tolerate therapy without complications.
Discussion: The treatment for most fistulas require surgical resection along with medical therapy. When patients are in remission from CD, the likelihood of developing fistulas is significantly decreased compared to those not in remission.

Figure: A) Image obtained during colonoscopy demonstrating poor bowel preparation of the transverse colon.
B) Image obtained during colonoscopy demonstrating fistula in the sigmoid colon.
C) Image obtained during colonoscopy demonstrating good bowel preparation of the rectum.
B) Image obtained during colonoscopy demonstrating fistula in the sigmoid colon.
C) Image obtained during colonoscopy demonstrating good bowel preparation of the rectum.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Gabrielle Sanford indicated no relevant financial relationships.
J Casey Chapman: Abbvie – Consultant, Speakers Bureau. Janssen – Consultant, Speakers Bureau. Pfizer – Consultant, Speakers Bureau. Takeda – Consultant, Speakers Bureau.
Randee Kidder indicated no relevant financial relationships.
Jeremy Polman, DO, MS, MBA1, Gabrielle Sanford, MD2, J Casey Chapman, MD3, Randee Kidder, FNP4. E0424 - Poor Bowel Preparation or Ileosigmoid Fistula: An Interesting Complication of Fistulizing Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
