Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0028 - A Delayed Diagnosis of a Functional Gastrinoma Mistaken for Atypical Crohn’s Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Mark Patrick Cubillan, MD
Zucker School of Medicine at Hofstra/Northwell Northshore and Long Island Jewish Hospital
Manhasset, NY
Presenting Author(s)
Mark Patrick Cubillan, MD1, Kara L. Raphael, MD2
1Zucker School of Medicine at Hofstra/Northwell Northshore and Long Island Jewish Hospital, Manhasset, NY; 2Zucker School of Medicine at Hofstra/Northwell, Northwell Health, North Shore University Hospital, Great Neck, NY
Introduction: Abdominal pain, vomiting, and diarrhea are cardinal symptoms of many GI diseases. A careful diagnostic workup is often necessary to find the etiology of the symptoms. Here, we present a patient with these symptoms whose diagnostic course was protracted but ultimately successful.
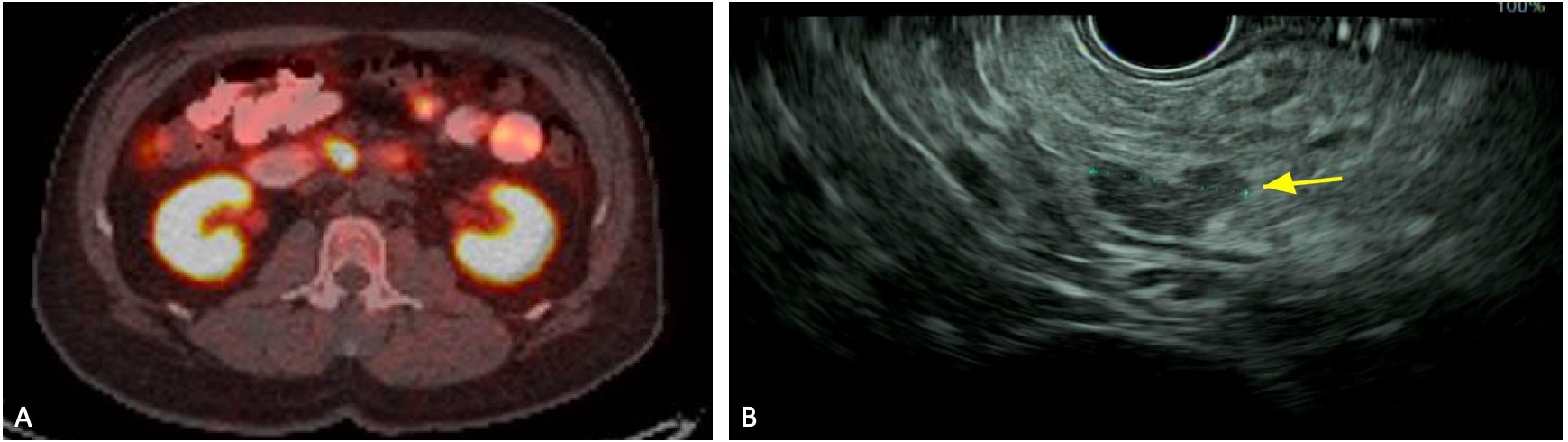
Case Description/Methods: A healthy 61yo man was admitted for 5 days of intractable diarrhea, vomiting and severe epigastric pain. Routine bloodwork was normal and CT showed nonspecific thickening in the stomach and small bowel without lesions. He was treated for viral gastroenteritis. However, his symptoms recurred. An MRI was normal without lesions. Colonoscopy was normal and push enteroscopy revealed esophagitis and multiple duodenal and jejunal ulcers. Biopsies showed focal acute jejunitis and erosion, suspicious for atypical Crohn’s disease. CRP was 92 and fecal calprotectin was 409, further supporting this diagnosis. A gastrin level was 707, felt to be due to PPI use. He was planned for Crohn’s treatment but did not start due to frequent ER visits for his symptoms that were treated conservatively. After 4 months, the patient was re-evaluated. He had an elevated chromogranin A of 2569. A DOTATATE PET was obtained given previous negative imaging and revealed increased uptake in the proximal pancreas and in the third portion of the duodenum (FIGURE A). EUS showed a 14mm pancreatic uncinate lesion (FIGURE B). FNB showed a low-grade neuroendocrine tumor (NET). He was diagnosed with a functional gastrinoma. He underwent a Whipple without complications and on follow up, his symptoms had completely resolved.
Discussion: This is a case of a delayed diagnosis of a functional gastrinoma causing persistent abdominal pain, vomiting and diarrhea. NETs are rare, found in 3/1,000,000 people, and only 10% are functional tumors. The diagnosis of a NET requires specific blood tests, visible lesions, and positive biopsies. Here, the patient’s initial evaluation was indeterminant for NET and biopsies suggested Crohn’s, delaying his correct diagnosis and treatment. CT and MRI have poor sensitivities (59% and 20%) for detection of gastrinomas without hepatic metastases. However, DOTATATE PETs have a detection rate of 92% in patients with equivocal CTs. EUS has a high sensitivity of 77% for pancreatic tumors. Thus, for patients with common and protracted symptoms, the differential diagnosis should remain broad, and further investigation with higher yield tests may be necessary to arrive at a timely diagnosis and treatment.
Disclosures:
Mark Patrick Cubillan, MD1, Kara L. Raphael, MD2. E0028 - A Delayed Diagnosis of a Functional Gastrinoma Mistaken for Atypical Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Zucker School of Medicine at Hofstra/Northwell Northshore and Long Island Jewish Hospital, Manhasset, NY; 2Zucker School of Medicine at Hofstra/Northwell, Northwell Health, North Shore University Hospital, Great Neck, NY
Introduction: Abdominal pain, vomiting, and diarrhea are cardinal symptoms of many GI diseases. A careful diagnostic workup is often necessary to find the etiology of the symptoms. Here, we present a patient with these symptoms whose diagnostic course was protracted but ultimately successful.
Case Description/Methods: A healthy 61yo man was admitted for 5 days of intractable diarrhea, vomiting and severe epigastric pain. Routine bloodwork was normal and CT showed nonspecific thickening in the stomach and small bowel without lesions. He was treated for viral gastroenteritis. However, his symptoms recurred. An MRI was normal without lesions. Colonoscopy was normal and push enteroscopy revealed esophagitis and multiple duodenal and jejunal ulcers. Biopsies showed focal acute jejunitis and erosion, suspicious for atypical Crohn’s disease. CRP was 92 and fecal calprotectin was 409, further supporting this diagnosis. A gastrin level was 707, felt to be due to PPI use. He was planned for Crohn’s treatment but did not start due to frequent ER visits for his symptoms that were treated conservatively. After 4 months, the patient was re-evaluated. He had an elevated chromogranin A of 2569. A DOTATATE PET was obtained given previous negative imaging and revealed increased uptake in the proximal pancreas and in the third portion of the duodenum (FIGURE A). EUS showed a 14mm pancreatic uncinate lesion (FIGURE B). FNB showed a low-grade neuroendocrine tumor (NET). He was diagnosed with a functional gastrinoma. He underwent a Whipple without complications and on follow up, his symptoms had completely resolved.
Discussion: This is a case of a delayed diagnosis of a functional gastrinoma causing persistent abdominal pain, vomiting and diarrhea. NETs are rare, found in 3/1,000,000 people, and only 10% are functional tumors. The diagnosis of a NET requires specific blood tests, visible lesions, and positive biopsies. Here, the patient’s initial evaluation was indeterminant for NET and biopsies suggested Crohn’s, delaying his correct diagnosis and treatment. CT and MRI have poor sensitivities (59% and 20%) for detection of gastrinomas without hepatic metastases. However, DOTATATE PETs have a detection rate of 92% in patients with equivocal CTs. EUS has a high sensitivity of 77% for pancreatic tumors. Thus, for patients with common and protracted symptoms, the differential diagnosis should remain broad, and further investigation with higher yield tests may be necessary to arrive at a timely diagnosis and treatment.
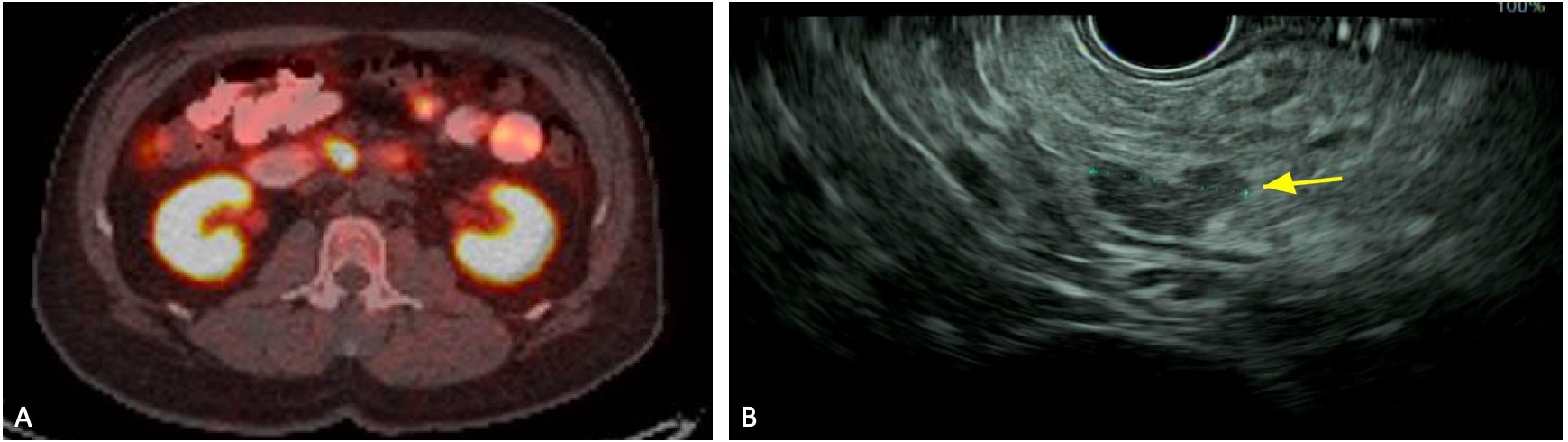
Figure: FIGURE A: DOTATATE PET Scan demonstrating increased FDG uptake at the 3rd portion of the duodenum.
FIGURE B: Endoscopic ultrasound demonstrating a 14mm pancreatic uncinate lesion.
FIGURE B: Endoscopic ultrasound demonstrating a 14mm pancreatic uncinate lesion.
Disclosures:
Mark Patrick Cubillan indicated no relevant financial relationships.
Kara Raphael indicated no relevant financial relationships.
Mark Patrick Cubillan, MD1, Kara L. Raphael, MD2. E0028 - A Delayed Diagnosis of a Functional Gastrinoma Mistaken for Atypical Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

