Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0031 - Acute Pancreatitis: Caused by Dislodged PEG Tube?
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Usama Sakhawat, MD
JOHNSON CITY, NY
Presenting Author(s)
Bhavani G. Murugesan, 1, Usama Sakhawat, MD2, Minhaz Ahmad, MD3, Fahad Malik, MD4, Nabih El Jundi, MD5, Catherine Spivak, 6, Nazif Chowdhury, MD3, Ali Marhaba, MD7
1SUNY Upstate, Johnson City, NY; 2United Health Services Hospitals, Johnson City, NY; 3United Health Services Hospital, Johnson City, NY; 4United Health Services- Wilson Hospital, Binghamton, NY; 5United Health Services, Johnson City, NY; 6SUNY Upstate Medical University, Syracuse, NY; 7United Health Services, Binghamton, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a common endoscopic procedure and a preferred route for long-term enteral nutrition for patients incapable of oral intake or for whom oral intake is insufficient. The insertion of PEG tubes is a relatively safe procedure with complications which include bleeding, aspiration, perforation, periostomal leaks, tube dislodgement and occlusion, gastric outlet obstruction due to tube migration and accidental removal. Acute pancreatitis secondary to PEG migration is rare. We present a patient with acute pancreatitis secondary to PEG tube migration.
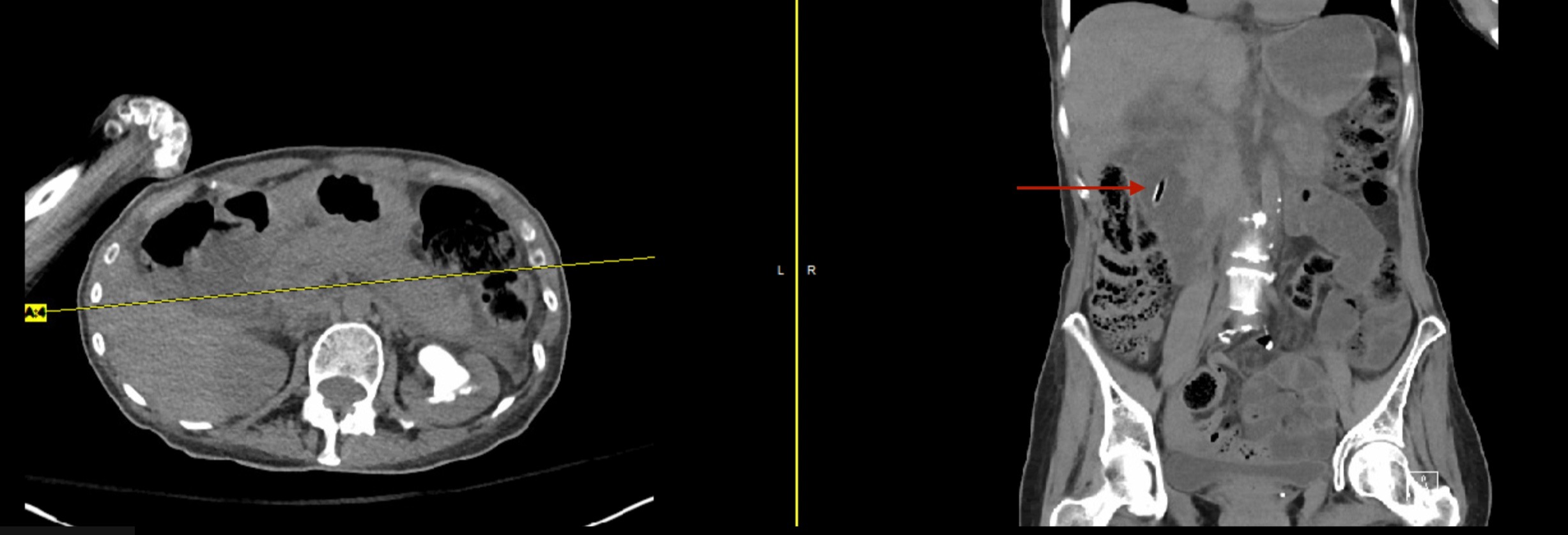
Case Description/Methods: A 57 year old woman known to have severe developmental delays, seizure disorder, bipolar 1 disorder presented with nausea, vomiting and abdominal pain. She is bedridden and nonverbal at baseline. She gets nutrition through a PEG tube for severe oropharyngeal dysphagia. Abdominal examination revealed significant biliary drainage from the gastrostomy site and tenderness present without rigidity or guarding. Labs showed WBC of 17.7 and lipase levels greater than 4,000 U/L. AST, ALT, alkaline phosphatase and total bilirubin were within normal range (31, 6, 94 and 0.9 respectively). CT abdomen without IV contrast revealed peripancreatic soft tissue stranding and pancreatic edema, the tip of the PEG tube in the second part of the duodenum (Figure 1). Her home medications are verified and are not known to cause acute pancreatitis (AP). So she was suspected to have AP from PEG tube migration. The tube was repositioned and she was treated with Ringer lactate. Four days later, her symptoms resolved and lipase level was within normal range (282 U/L).
Discussion: In comparison to other methods, enteral feeding has the benefit of maintaining gut mucosal integrity and decreasing the possibility for bacterial translocation. Migration of the PEG tube has been associated with gastric outlet obstruction and biliary obstruction. In rare cases, this can present as AP either through ampullary obstruction at the second part of the duodenum or through compression of the pancreatic head itself. This case highlights the inclusion of PEG tube induced pancreatitis as a differential for AP in patients receiving enteral feeding. Proper placement of the tube, regular examination of the site and marking the PEG position can help avoid migration and complications. The treatment for acute pancreatitis secondary to PEG tube migration is PEG tube removal followed by placement of a new PEG tube or repositioning.
Disclosures:
Bhavani G. Murugesan,1, Usama Sakhawat, MD2, Minhaz Ahmad, MD3, Fahad Malik, MD4, Nabih El Jundi, MD5, Catherine Spivak, 6, Nazif Chowdhury, MD3, Ali Marhaba, MD7. E0031 - Acute Pancreatitis: Caused by Dislodged PEG Tube?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1SUNY Upstate, Johnson City, NY; 2United Health Services Hospitals, Johnson City, NY; 3United Health Services Hospital, Johnson City, NY; 4United Health Services- Wilson Hospital, Binghamton, NY; 5United Health Services, Johnson City, NY; 6SUNY Upstate Medical University, Syracuse, NY; 7United Health Services, Binghamton, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a common endoscopic procedure and a preferred route for long-term enteral nutrition for patients incapable of oral intake or for whom oral intake is insufficient. The insertion of PEG tubes is a relatively safe procedure with complications which include bleeding, aspiration, perforation, periostomal leaks, tube dislodgement and occlusion, gastric outlet obstruction due to tube migration and accidental removal. Acute pancreatitis secondary to PEG migration is rare. We present a patient with acute pancreatitis secondary to PEG tube migration.
Case Description/Methods: A 57 year old woman known to have severe developmental delays, seizure disorder, bipolar 1 disorder presented with nausea, vomiting and abdominal pain. She is bedridden and nonverbal at baseline. She gets nutrition through a PEG tube for severe oropharyngeal dysphagia. Abdominal examination revealed significant biliary drainage from the gastrostomy site and tenderness present without rigidity or guarding. Labs showed WBC of 17.7 and lipase levels greater than 4,000 U/L. AST, ALT, alkaline phosphatase and total bilirubin were within normal range (31, 6, 94 and 0.9 respectively). CT abdomen without IV contrast revealed peripancreatic soft tissue stranding and pancreatic edema, the tip of the PEG tube in the second part of the duodenum (Figure 1). Her home medications are verified and are not known to cause acute pancreatitis (AP). So she was suspected to have AP from PEG tube migration. The tube was repositioned and she was treated with Ringer lactate. Four days later, her symptoms resolved and lipase level was within normal range (282 U/L).
Discussion: In comparison to other methods, enteral feeding has the benefit of maintaining gut mucosal integrity and decreasing the possibility for bacterial translocation. Migration of the PEG tube has been associated with gastric outlet obstruction and biliary obstruction. In rare cases, this can present as AP either through ampullary obstruction at the second part of the duodenum or through compression of the pancreatic head itself. This case highlights the inclusion of PEG tube induced pancreatitis as a differential for AP in patients receiving enteral feeding. Proper placement of the tube, regular examination of the site and marking the PEG position can help avoid migration and complications. The treatment for acute pancreatitis secondary to PEG tube migration is PEG tube removal followed by placement of a new PEG tube or repositioning.
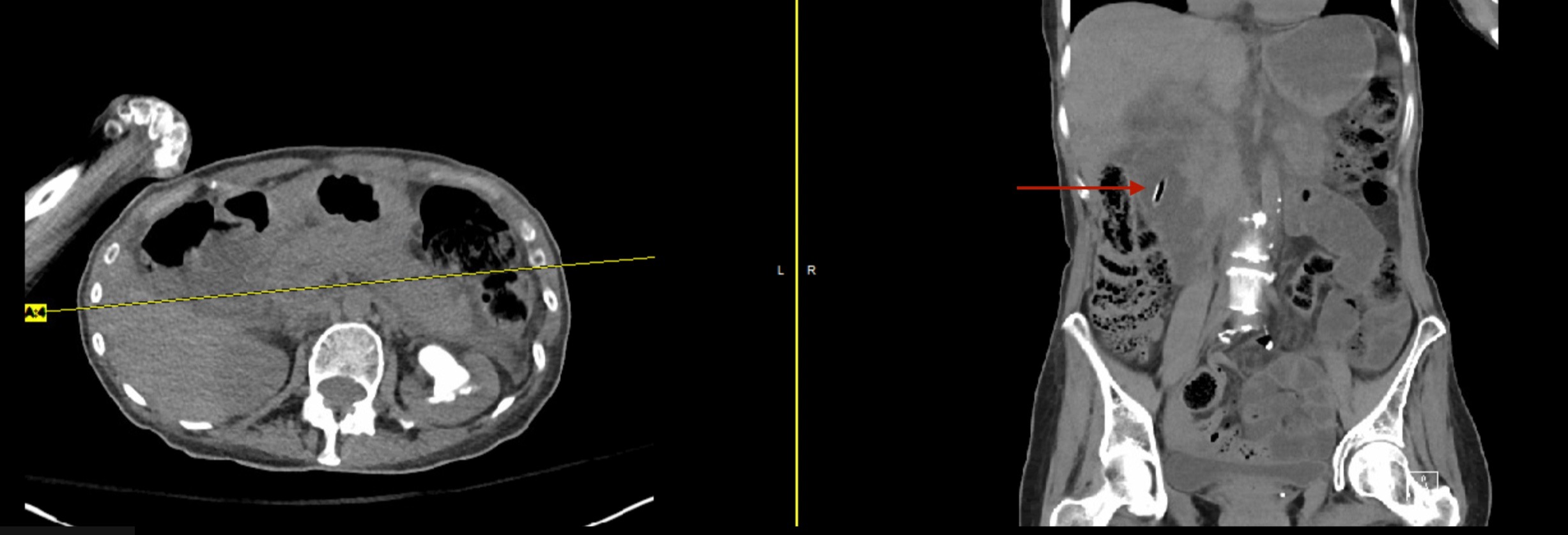
Figure: Peripancreatic soft tissue stranding and pancreatic edema, the tip of the PEG tube in the second part of the duodenum.
Disclosures:
Bhavani Murugesan indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Minhaz Ahmad indicated no relevant financial relationships.
Fahad Malik indicated no relevant financial relationships.
Nabih El Jundi indicated no relevant financial relationships.
Catherine Spivak indicated no relevant financial relationships.
Nazif Chowdhury indicated no relevant financial relationships.
Ali Marhaba indicated no relevant financial relationships.
Bhavani G. Murugesan,1, Usama Sakhawat, MD2, Minhaz Ahmad, MD3, Fahad Malik, MD4, Nabih El Jundi, MD5, Catherine Spivak, 6, Nazif Chowdhury, MD3, Ali Marhaba, MD7. E0031 - Acute Pancreatitis: Caused by Dislodged PEG Tube?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
