Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0036 - Hemorrhagic Cholecystitis: A Rare Cause of Brisk Upper Gastrointestinal Bleeding
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- NJ
Neil R. Jariwalla, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Neil R. Jariwalla, MD1, Samuel S. Ji, DO1, David Cheung, MD2, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3
1University of California Irvine, Orange, CA; 2UCI Medical Center, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Gastrointestinal bleeding is a commonly seen problem in the hospital and timely identification of the source is important in brisk bleeds to allow for prompt interventions. Unfortunately, the cause of the bleeding can sometimes be difficult to identify and can require thinking outside the box. We present a rare case of hemorrhagic cholecystitis manifesting as hematochezia and hypotension in the setting of chronic liver disease.
Case Description/Methods: A 55-year-old man with history of alcoholic cirrhosis (Meld-Na 24, Child-Pugh C) initially presented to an outside hospital with one week of nausea, vomiting, abdominal pain and watery diarrhea in the setting of alcohol withdrawal.
He underwent an esophagogastroduodenoscopy (EGD) revealing a single gastric varix with red nipple without active bleeding and no esophageal varices. His liver function began to worsen and improved with supportive care. His improvement interestingly correlated with acute onset of hematochezia. A repeat EGD and colonoscopy revealed numerous blood clots in the colon without an active source of bleeding. He was transferred to our academic medical center for higher level of care.
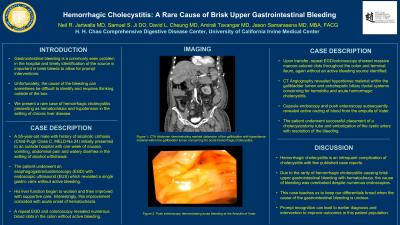
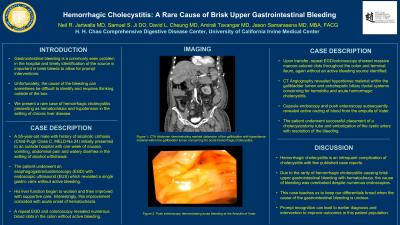
Upon arrival, he continued to have hematemesis and hematochezia. Repeat EGD/colonoscopy showed small non-bleeding gastric varices as well as massive maroon-colored clots throughout the colon and terminal ileum but no signs of active bleeding. CT angiography (CTA) revealed hyperdense material within the gallbladder lumen and extrahepatic biliary ductal systems suspicious for hemobilia and acute hemorrhagic cholecystitis. Pt underwent capsule endoscopy revealing an irregular oozing of blood in the proximal small intestine. A push enteroscopy then revealed actively oozing blood from the ampulla of Vater. Patient subsequently underwent successful cholecystostomy tube placement and cystic artery embolization with resolution of his bleeding.
Discussion: Hemorrhagic cholecystitis is an infrequent complication of cholecystitis with few published case reports. Due to the rarity of hemorrhagic cholecystitis causing brisk upper gastrointestinal bleeding with hematochezia, the cause of the bleeding was overlooked despite numerous endoscopies and not found until a capsule endoscopy was performed. This case teaches us to keep our differentials broad when the cause of the gastrointestinal bleeding is unclear. Prompt recognition can lead to earlier diagnosis and intervention to improve outcomes in this patient population.

Disclosures:
Neil R. Jariwalla, MD1, Samuel S. Ji, DO1, David Cheung, MD2, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3. E0036 - Hemorrhagic Cholecystitis: A Rare Cause of Brisk Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2UCI Medical Center, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Gastrointestinal bleeding is a commonly seen problem in the hospital and timely identification of the source is important in brisk bleeds to allow for prompt interventions. Unfortunately, the cause of the bleeding can sometimes be difficult to identify and can require thinking outside the box. We present a rare case of hemorrhagic cholecystitis manifesting as hematochezia and hypotension in the setting of chronic liver disease.
Case Description/Methods: A 55-year-old man with history of alcoholic cirrhosis (Meld-Na 24, Child-Pugh C) initially presented to an outside hospital with one week of nausea, vomiting, abdominal pain and watery diarrhea in the setting of alcohol withdrawal.
He underwent an esophagogastroduodenoscopy (EGD) revealing a single gastric varix with red nipple without active bleeding and no esophageal varices. His liver function began to worsen and improved with supportive care. His improvement interestingly correlated with acute onset of hematochezia. A repeat EGD and colonoscopy revealed numerous blood clots in the colon without an active source of bleeding. He was transferred to our academic medical center for higher level of care.
Upon arrival, he continued to have hematemesis and hematochezia. Repeat EGD/colonoscopy showed small non-bleeding gastric varices as well as massive maroon-colored clots throughout the colon and terminal ileum but no signs of active bleeding. CT angiography (CTA) revealed hyperdense material within the gallbladder lumen and extrahepatic biliary ductal systems suspicious for hemobilia and acute hemorrhagic cholecystitis. Pt underwent capsule endoscopy revealing an irregular oozing of blood in the proximal small intestine. A push enteroscopy then revealed actively oozing blood from the ampulla of Vater. Patient subsequently underwent successful cholecystostomy tube placement and cystic artery embolization with resolution of his bleeding.
Discussion: Hemorrhagic cholecystitis is an infrequent complication of cholecystitis with few published case reports. Due to the rarity of hemorrhagic cholecystitis causing brisk upper gastrointestinal bleeding with hematochezia, the cause of the bleeding was overlooked despite numerous endoscopies and not found until a capsule endoscopy was performed. This case teaches us to keep our differentials broad when the cause of the gastrointestinal bleeding is unclear. Prompt recognition can lead to earlier diagnosis and intervention to improve outcomes in this patient population.

Figure: Enteroscopy demonstrating bleeding at the Ampulla of Vater.
Disclosures:
Neil Jariwalla indicated no relevant financial relationships.
Samuel Ji indicated no relevant financial relationships.
David Cheung indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Jason Samarasena: Conmed – Consultant. Docbot – Stock Options. Mauna Kea – Consultant. Olympus – Consultant. Ovesco – Consultant. Steris – Consultant.
Neil R. Jariwalla, MD1, Samuel S. Ji, DO1, David Cheung, MD2, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3. E0036 - Hemorrhagic Cholecystitis: A Rare Cause of Brisk Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
