Back

Poster Session D - Tuesday Morning
Category: IBD
D0364 - Association of Serum IgG4 and Disease Outcomes in Patients with Inflammatory Bowel Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

R. Christopher Chase, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
R. Christopher Chase, MD1, Hani Tamim, PhD2, Kristin Clift, MA1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc3, David H. Bruining, MD4, Christina Ha, MD5
1Mayo Clinic, Jacksonville, FL; 2American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon; 3Mayo Clinic Florida, Jacksonville, FL; 4Mayo Clinic, Rochester, MN; 5Mayo Clinic, Scottsdale, AZ
Introduction: The etiology of Inflammatory bowel disease (IBD) is multifactorial and is thought to be influenced by inappropriate activation of the gut mucosal immune system. Immunoglobulin G (IgG) humoral immune response specifically subclasses 1, 2, & 3 activate the classical complement pathway to clear infection. IgG subclass 4 (IgG4) cannot activate the classical complement cascade. The role of IgG4 in IBD pathophysiology as an immunomodulator is controversial. This study aims to characterize the association of low, normal, and high IgG4 levels on the outcomes of patients with IBD.
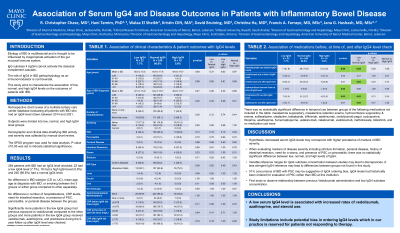
Methods: This was a retrospective chart review of a multisite tertiary care center database evaluating all patients with IBD who had an IgG4 level drawn between 2014 and 2021. Subjects were divided into low, normal, and high IgG4 level groups. Demographic and clinical data stratifying IBD activity and severity was collected by manual chart review. The SPSS program was used for data analysis. Categorical variables were summarized using the number and percent, and continuous variables were summarized by mean and standard deviation. Associations were done using the chi-square or Fishers exact test for categorical variables, and ANOVA or Mann Whitney for continuous variables. P-value of 0.05 was set to indicate statistical significance.
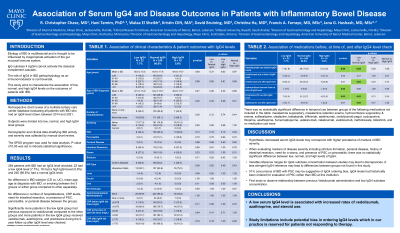
Results: 284 patients with IBD had an IgG4 level checked. Of these patients, 22 had a low IgG4 level (7.7%), 16 had a high IgG4 level (5.6%) and 246 (86.6%) had a normal IgG4 level. There was no difference in IBD subtype (Crohn’s disease vs. ulcerative colitis), mean age, age at diagnosis with IBD, or smoking between the 3 groups or either group compared to the other separately. There was no difference in number of hospitalizations, C-reactive protein levels, need for intestinal resection, or in presence of primary sclerosing cholangitis, pancreatitis, or perianal disease between the groups. Regarding medication use, significantly more patients in the low IgG4 group had previous exposure to vedolizumab compared to the other groups and more patients in the low IgG4 group received vedolizumab, azathioprine, and prednisone during the 5-year follow up after IgG4 level was checked.
Discussion: A low serum IgG4 level is associated with increased rates of vedolizumab, azathioprine, and steroid use. Study limitations include potential bias in ordering IgG4 levels which in our practice is reserved for patients not responding to therapy.
Disclosures:
R. Christopher Chase, MD1, Hani Tamim, PhD2, Kristin Clift, MA1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc3, David H. Bruining, MD4, Christina Ha, MD5. D0364 - Association of Serum IgG4 and Disease Outcomes in Patients with Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon; 3Mayo Clinic Florida, Jacksonville, FL; 4Mayo Clinic, Rochester, MN; 5Mayo Clinic, Scottsdale, AZ
Introduction: The etiology of Inflammatory bowel disease (IBD) is multifactorial and is thought to be influenced by inappropriate activation of the gut mucosal immune system. Immunoglobulin G (IgG) humoral immune response specifically subclasses 1, 2, & 3 activate the classical complement pathway to clear infection. IgG subclass 4 (IgG4) cannot activate the classical complement cascade. The role of IgG4 in IBD pathophysiology as an immunomodulator is controversial. This study aims to characterize the association of low, normal, and high IgG4 levels on the outcomes of patients with IBD.
Methods: This was a retrospective chart review of a multisite tertiary care center database evaluating all patients with IBD who had an IgG4 level drawn between 2014 and 2021. Subjects were divided into low, normal, and high IgG4 level groups. Demographic and clinical data stratifying IBD activity and severity was collected by manual chart review. The SPSS program was used for data analysis. Categorical variables were summarized using the number and percent, and continuous variables were summarized by mean and standard deviation. Associations were done using the chi-square or Fishers exact test for categorical variables, and ANOVA or Mann Whitney for continuous variables. P-value of 0.05 was set to indicate statistical significance.
Results: 284 patients with IBD had an IgG4 level checked. Of these patients, 22 had a low IgG4 level (7.7%), 16 had a high IgG4 level (5.6%) and 246 (86.6%) had a normal IgG4 level. There was no difference in IBD subtype (Crohn’s disease vs. ulcerative colitis), mean age, age at diagnosis with IBD, or smoking between the 3 groups or either group compared to the other separately. There was no difference in number of hospitalizations, C-reactive protein levels, need for intestinal resection, or in presence of primary sclerosing cholangitis, pancreatitis, or perianal disease between the groups. Regarding medication use, significantly more patients in the low IgG4 group had previous exposure to vedolizumab compared to the other groups and more patients in the low IgG4 group received vedolizumab, azathioprine, and prednisone during the 5-year follow up after IgG4 level was checked.
Discussion: A low serum IgG4 level is associated with increased rates of vedolizumab, azathioprine, and steroid use. Study limitations include potential bias in ordering IgG4 levels which in our practice is reserved for patients not responding to therapy.
Disclosures:
R. Christopher Chase indicated no relevant financial relationships.
Hani Tamim indicated no relevant financial relationships.
Kristin Clift indicated no relevant financial relationships.
Francis Farraye: Adiso Therapeutics – DSMB. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. GSK – Advisory Committee/Board Member. IBD Educational Group – Advisory Committee/Board Member. Innovation Pharmaceuticals – Stock Options. Iterative Scopes – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Theravance – DSMB.
Jana Hashash indicated no relevant financial relationships.
David Bruining: Janssen – Advisory Committee/Board Member. Medtronic – Grant/Research Support. Takeda – Grant/Research Support.
Christina Ha: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member. Index Pharmaceuticals – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Takeda – Advisory Committee/Board Member.
R. Christopher Chase, MD1, Hani Tamim, PhD2, Kristin Clift, MA1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc3, David H. Bruining, MD4, Christina Ha, MD5. D0364 - Association of Serum IgG4 and Disease Outcomes in Patients with Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
