Back

Poster Session C - Monday Afternoon
Category: Stomach
C0704 - Disguised as Post-Operative Ileus: A Case of a Giant Gastric Ulcer Causing Outlet Obstruction and Gastric Pneumatosis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Natasha Narang, DO
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Natasha Narang, DO, Nael Haddad, MD, Mahmoud Bayoumi, MD, MPH, Victor Arce Gutierrez, MD, Paul Gomez, MD, Hugo Pinillos, MD, FACG
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Giant gastric ulcers (GGU), defined as ulcers larger than 2-3cm, are relatively rare in the setting of widespread proton pump inhibitor (PPI) use. Though usually located in the lesser curvature, GGU may occur in any part of the stomach. Typical symptoms are similar to that of peptic ulcer disease (PUD), i.e. epigastric pain and gastrointestinal bleeding, however GGU are highly prone to perforation and are more likely to be malignant in the elderly. Overall, gastric outlet obstruction is the least common complication of PUD.
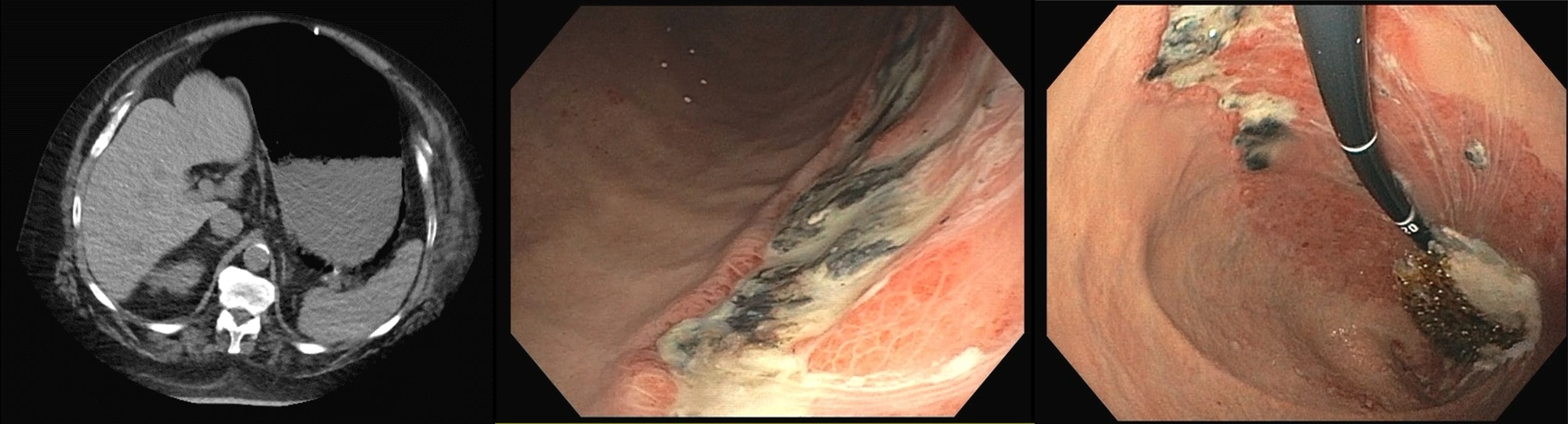
Case Description/Methods: A 74-year-old obese male with history diabetes, sleep apnea, and prior laparoscopic gastric banding surgery was admitted for elective surgery for Charcot arthropathy. Post-operatively, he developed nausea, vomiting and abdominal bloating. Abdominal x-ray showed distention of the small bowel concerning for ileus. Exam showed a non-tender abdomen with distention and tympany on percussion. His emesis resolved with antiemetics, however distention persisted despite passing gas and stool. Three days after surgery, he developed acute anemia without overt bleeding requiring blood transfusions. Abdominal X-ray and CT was performed which showed marked gaseous distention of the stomach and gastric wall pneumatosis. Nasogastric tube was placed for decompression with subsequent resolution of his distention. Due to concern for gastric band erosion, Gastroenterology was consulted. Upper endoscopy was performed which revealed a 4cm clean-based ulcer with overlaying eschar along the greater curvature with surrounding erythema and edema. Biopsies of the ulcer border showed acute erosive gastropathy with focal clustering of eosinophils without evidence of dysplasia. He was started on PPI and sucralfate, and remained clinically stable without further gastrointestinal symptoms.
Discussion: Gastric pneumatosis due to gastric emphysema is caused by disruption of mucosa leading to air migrating into the gastric wall. Etiologies vary, including injury from instrumentation, severe vomiting, pulmonary pathology, penetrating gastric ulcers, or gastric outlet obstruction. Few cases reports have described gastric emphysema resulting from gastric band erosion, however there are no reports describing this occurring in the absence of full erosion. Overall, gastric emphysema is relatively rare, as is development of GGU. To our knowledge, this is the first reported case of unperforated giant gastric ulcer resulting in outlet obstruction with gastric pneumatosis.
Disclosures:
Natasha Narang, DO, Nael Haddad, MD, Mahmoud Bayoumi, MD, MPH, Victor Arce Gutierrez, MD, Paul Gomez, MD, Hugo Pinillos, MD, FACG. C0704 - Disguised as Post-Operative Ileus: A Case of a Giant Gastric Ulcer Causing Outlet Obstruction and Gastric Pneumatosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Giant gastric ulcers (GGU), defined as ulcers larger than 2-3cm, are relatively rare in the setting of widespread proton pump inhibitor (PPI) use. Though usually located in the lesser curvature, GGU may occur in any part of the stomach. Typical symptoms are similar to that of peptic ulcer disease (PUD), i.e. epigastric pain and gastrointestinal bleeding, however GGU are highly prone to perforation and are more likely to be malignant in the elderly. Overall, gastric outlet obstruction is the least common complication of PUD.
Case Description/Methods: A 74-year-old obese male with history diabetes, sleep apnea, and prior laparoscopic gastric banding surgery was admitted for elective surgery for Charcot arthropathy. Post-operatively, he developed nausea, vomiting and abdominal bloating. Abdominal x-ray showed distention of the small bowel concerning for ileus. Exam showed a non-tender abdomen with distention and tympany on percussion. His emesis resolved with antiemetics, however distention persisted despite passing gas and stool. Three days after surgery, he developed acute anemia without overt bleeding requiring blood transfusions. Abdominal X-ray and CT was performed which showed marked gaseous distention of the stomach and gastric wall pneumatosis. Nasogastric tube was placed for decompression with subsequent resolution of his distention. Due to concern for gastric band erosion, Gastroenterology was consulted. Upper endoscopy was performed which revealed a 4cm clean-based ulcer with overlaying eschar along the greater curvature with surrounding erythema and edema. Biopsies of the ulcer border showed acute erosive gastropathy with focal clustering of eosinophils without evidence of dysplasia. He was started on PPI and sucralfate, and remained clinically stable without further gastrointestinal symptoms.
Discussion: Gastric pneumatosis due to gastric emphysema is caused by disruption of mucosa leading to air migrating into the gastric wall. Etiologies vary, including injury from instrumentation, severe vomiting, pulmonary pathology, penetrating gastric ulcers, or gastric outlet obstruction. Few cases reports have described gastric emphysema resulting from gastric band erosion, however there are no reports describing this occurring in the absence of full erosion. Overall, gastric emphysema is relatively rare, as is development of GGU. To our knowledge, this is the first reported case of unperforated giant gastric ulcer resulting in outlet obstruction with gastric pneumatosis.
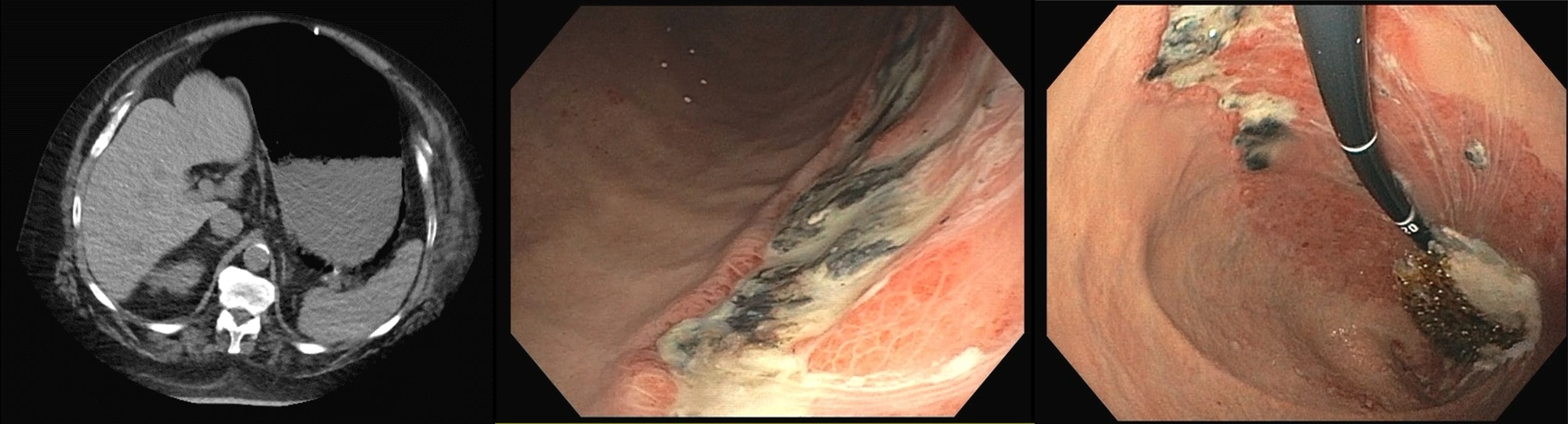
Figure: Figure 1. CT abdomen showing marked gaseous distention of the stomach and gastric wall pneumatosis (Figure 1a). Upper endoscopy findings of a friable, erythematous giant ulcer with clean-base overlaying the greater curvature with significant surrounding erythema and edema in the fundus/cardia (Figure 1b and 1c), as well as multiple surrounding small ulcerations, some with clean-base and some with flat pigmented spots, throughout (not pictured). No evidence of active bleeding, visible vessel, or high-risk features for bleeding.
Disclosures:
Natasha Narang indicated no relevant financial relationships.
Nael Haddad indicated no relevant financial relationships.
Mahmoud Bayoumi indicated no relevant financial relationships.
Victor Arce Gutierrez indicated no relevant financial relationships.
Paul Gomez indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Natasha Narang, DO, Nael Haddad, MD, Mahmoud Bayoumi, MD, MPH, Victor Arce Gutierrez, MD, Paul Gomez, MD, Hugo Pinillos, MD, FACG. C0704 - Disguised as Post-Operative Ileus: A Case of a Giant Gastric Ulcer Causing Outlet Obstruction and Gastric Pneumatosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
