Back

Poster Session C - Monday Afternoon
Category: Stomach
C0705 - A Unique Manifestation of Tuberculosis in the Gut
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sanjay Prasad, MD
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Sanjay Prasad, MD1, Natasha McMillan, MD2, Hari Sayana, MD3
1University of Texas Health Science Center, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3UT Health San Antonio, San Antonio, TX
Introduction: Abdominal manifestations of tuberculosis (TB) can involve the peritoneum, gastric body, intestinal tract, pancreas, perianal region, hepatobiliary region, and surrounding lymph nodes in patients with associated risk factors. We present a patient with known TB exposure and a gastric mass with associated lymphadenopathy (LAD), later determined to be secondary to gastric tuberculosis.
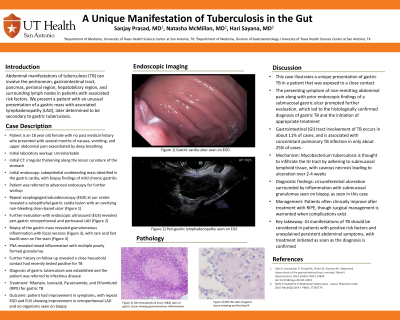
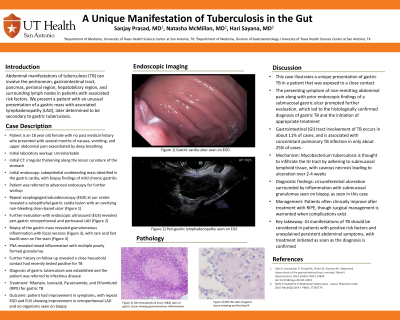
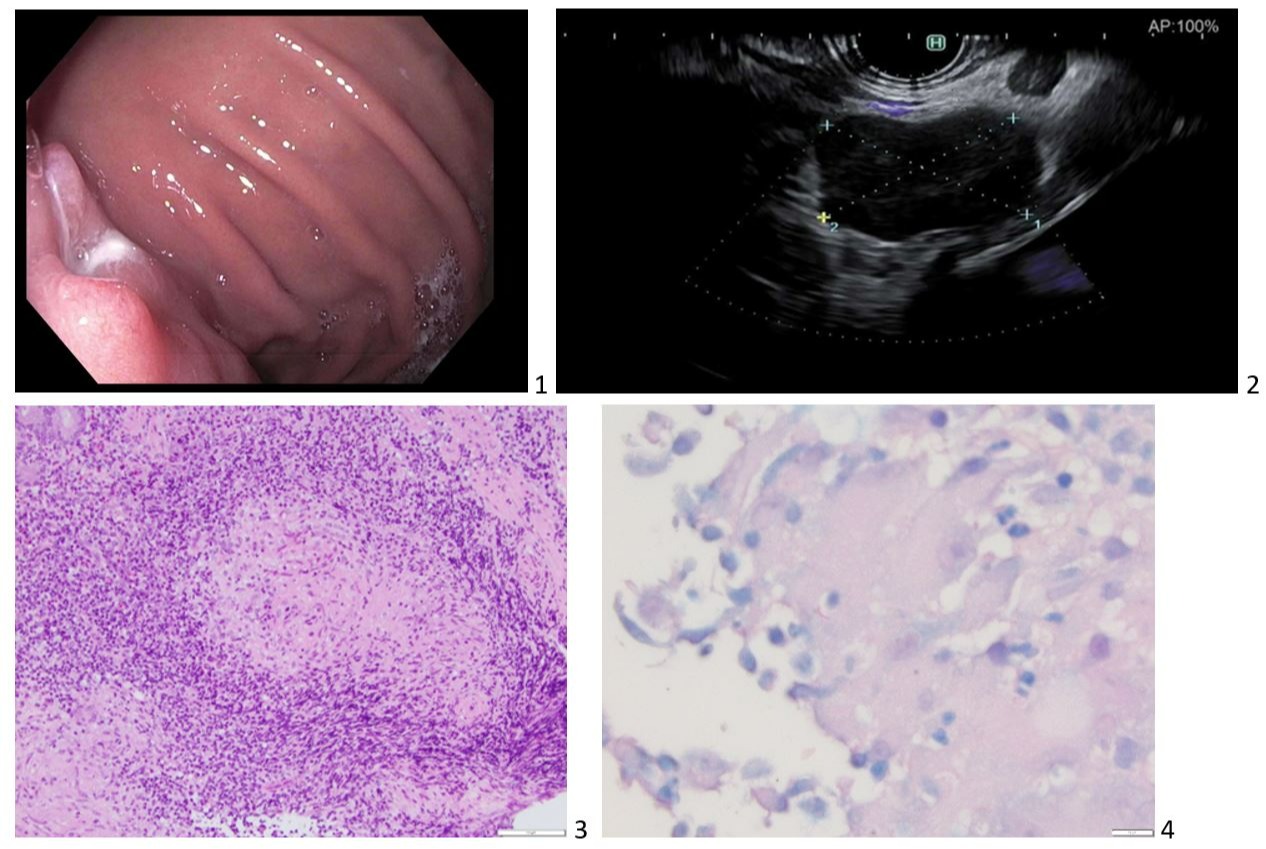
Case Description/Methods: An 18 year old female with no past medical history presented with several months of upper abdominal pain exacerbated by deep breathing. A prior esophagogastroduodenoscopy (EGD) revealed a submucosal gastric ulcer (1), and further evaluation with an EGD and endoscopic ultrasound (EUS) revealed a peri-gastric mass with retroperitoneal and portocaval LAD (2). Fine needle aspiration (FNA) of the mass revealed granulomatous inflammation with focal necrosis (3) and rare acid fast bacilli seen on Fite stain (4). Further history on follow up revealed a close household contact had recently tested positive for TB. The patient was started on full treatment with Rifampin, Isoniazid, Pyrazinamide, and Ethambutol (RIPE) for gastric TB, with improvement in symptoms noted on follow up. A repeat EGD with EUS was performed 7 months after the initial, with observed improvement in retroperitoneal LAD and no organisms seen on FNA.
Discussion: This case illustrates a unique presentation of gastric TB in a patient, later determined to have been exposed to a close contact. The presenting symptom of non-remitting abdominal pain along with prior endoscopic findings of a submucosal gastric ulcer prompted further evaluation, which led to the histologically confirmed diagnosis of gastric TB and the initiation of appropriate treatment. Gastrointestinal (GI) tract involvement of TB occurs in about 11% of cases, and is associated with concomitant pulmonary TB infection in only about 25% of cases. Mycobacterium tuberculosis is thought to infiltrate the GI tract by adhering to submucosal lymphoid tissue, with caseous necrosis leading to ulceration over 2-4 weeks. Diagnostic findings include circumferential ulceration surrounded by inflammation with submucosal granulomas seen on biopsy, as seen in this case. Patients often clinically improve after treatment with RIPE, though surgical management is warranted when complications exist. GI manifestations of TB should be considered in patients with positive risk factors and unexplained persistent abdominal symptoms, with treatment initiated as soon as the diagnosis is confirmed.
Disclosures:
Sanjay Prasad, MD1, Natasha McMillan, MD2, Hari Sayana, MD3. C0705 - A Unique Manifestation of Tuberculosis in the Gut, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Health Science Center, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3UT Health San Antonio, San Antonio, TX
Introduction: Abdominal manifestations of tuberculosis (TB) can involve the peritoneum, gastric body, intestinal tract, pancreas, perianal region, hepatobiliary region, and surrounding lymph nodes in patients with associated risk factors. We present a patient with known TB exposure and a gastric mass with associated lymphadenopathy (LAD), later determined to be secondary to gastric tuberculosis.
Case Description/Methods: An 18 year old female with no past medical history presented with several months of upper abdominal pain exacerbated by deep breathing. A prior esophagogastroduodenoscopy (EGD) revealed a submucosal gastric ulcer (1), and further evaluation with an EGD and endoscopic ultrasound (EUS) revealed a peri-gastric mass with retroperitoneal and portocaval LAD (2). Fine needle aspiration (FNA) of the mass revealed granulomatous inflammation with focal necrosis (3) and rare acid fast bacilli seen on Fite stain (4). Further history on follow up revealed a close household contact had recently tested positive for TB. The patient was started on full treatment with Rifampin, Isoniazid, Pyrazinamide, and Ethambutol (RIPE) for gastric TB, with improvement in symptoms noted on follow up. A repeat EGD with EUS was performed 7 months after the initial, with observed improvement in retroperitoneal LAD and no organisms seen on FNA.
Discussion: This case illustrates a unique presentation of gastric TB in a patient, later determined to have been exposed to a close contact. The presenting symptom of non-remitting abdominal pain along with prior endoscopic findings of a submucosal gastric ulcer prompted further evaluation, which led to the histologically confirmed diagnosis of gastric TB and the initiation of appropriate treatment. Gastrointestinal (GI) tract involvement of TB occurs in about 11% of cases, and is associated with concomitant pulmonary TB infection in only about 25% of cases. Mycobacterium tuberculosis is thought to infiltrate the GI tract by adhering to submucosal lymphoid tissue, with caseous necrosis leading to ulceration over 2-4 weeks. Diagnostic findings include circumferential ulceration surrounded by inflammation with submucosal granulomas seen on biopsy, as seen in this case. Patients often clinically improve after treatment with RIPE, though surgical management is warranted when complications exist. GI manifestations of TB should be considered in patients with positive risk factors and unexplained persistent abdominal symptoms, with treatment initiated as soon as the diagnosis is confirmed.
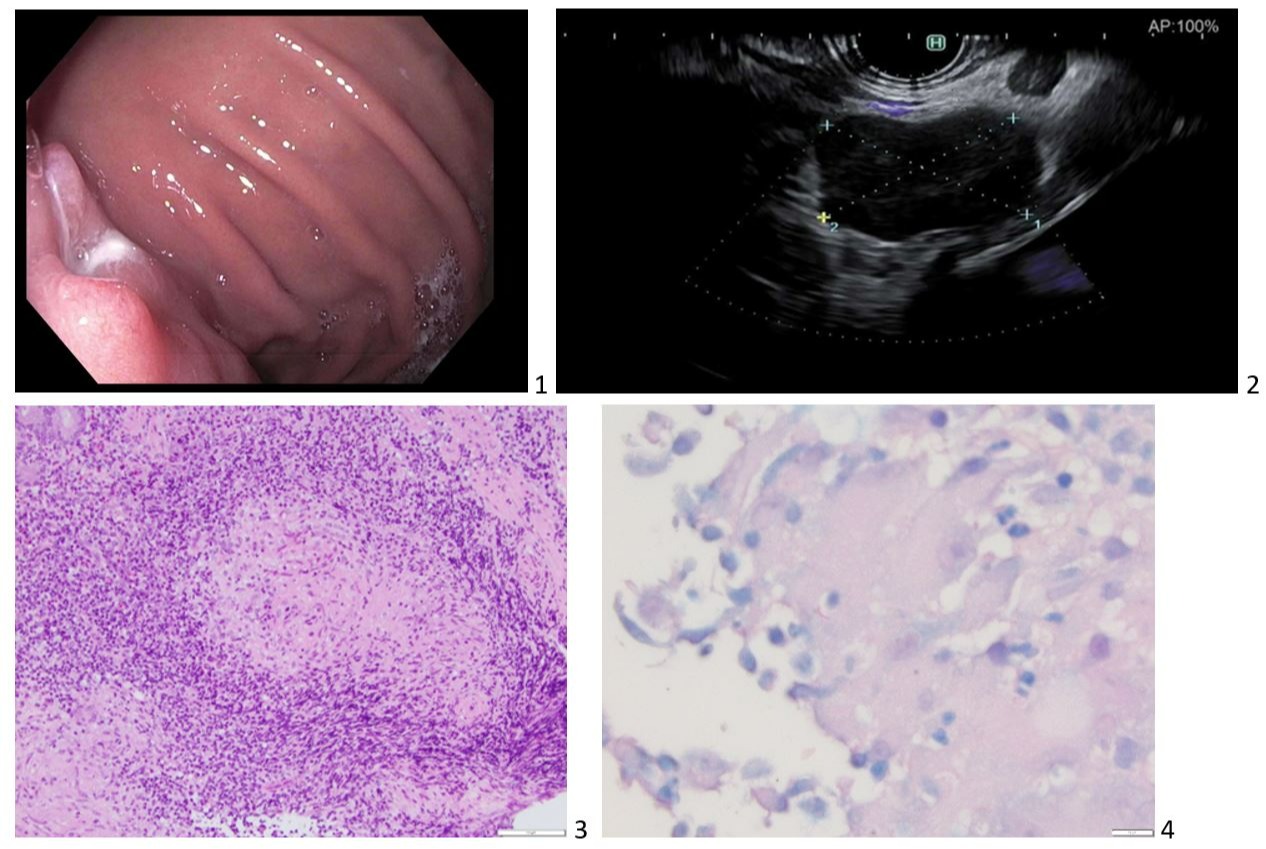
Figure: 1) Gastric cardia ulcer seen on EGD
2) Peri-gastric lymphadenopathy seen on EUS
3) 10x Hematoxylin & Eosin (H&E) stain of gastric tissue showing granulomatous inflammation
4) 60x Fite stain of gastric tissue showing acid fast bacilli
2) Peri-gastric lymphadenopathy seen on EUS
3) 10x Hematoxylin & Eosin (H&E) stain of gastric tissue showing granulomatous inflammation
4) 60x Fite stain of gastric tissue showing acid fast bacilli
Disclosures:
Sanjay Prasad indicated no relevant financial relationships.
Natasha McMillan indicated no relevant financial relationships.
Hari Sayana indicated no relevant financial relationships.
Sanjay Prasad, MD1, Natasha McMillan, MD2, Hari Sayana, MD3. C0705 - A Unique Manifestation of Tuberculosis in the Gut, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
