Back

Poster Session C - Monday Afternoon
Category: General Endoscopy
C0306 - Blanching Gastric Mucosa: An Endoscopic Finding in a Patient With Celiac Artery Occlusion Leading to Vascular Insufficiency
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Erika Vigandt, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Erika Vigandt, MD1, Denzil Etienne, MD1, Eric Landa, MD2
1The Brooklyn Hospital Center, Brooklyn, NY; 2Wyckoff Heights Medical Center, Brooklyn, NY
Introduction: Celiac artery occlusion is a significant and debilitating disorder usually characterized by abdominal pain and diagnosed via radiological imaging modalities. Endoscopic findings in this disease have not been clearly depicted. We present a case with significant endoscopic findings of patchy blanching gastric mucosa induced by insufflation during esophagogastroduodenoscopy (EGD).
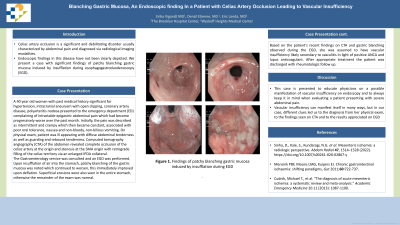
Case Description/Methods: A 40 year old woman with past medical history significant for hypertension, intracranial aneurysm with open clipping, coronary artery disease, polyarteritis nodosa presented to the emergency department (ED) complaining of intractable epigastric abdominal pain which had become progressively worse over the past month. Initially, the pain was described as intermittent and crampy which then became constant, 10/10 in intensity, associated with poor oral tolerance, nausea and non-bloody, non-bilious vomiting. Upon presentation vital signs were T 97.9 F, HR 96 bpm, BP 162/117 mmHg, SpO2 99% on room air. On physical exam, patient was ill appearing with diffuse abdominal tenderness with guarding and rebound tenderness, soft, non-distended, with bowel sounds appreciated. Computed tomography angiography (CTA) of the abdomen/pelvis revealed complete occlusion of the celiac artery at the origin and stenosis at the SMA origin with retrograde filling of the celiac territory via an enlarged IPDA collateral. The Gastroenterology service was consulted and an EGD was performed. Upon insufflation of air into the stomach, patchy blanching of the gastric mucosa was noted which continued to worsen, this immediately improved upon deflation. Superficial erosions were also seen in the entire stomach, otherwise the remainder of the exam was normal. Based on the patient’s recent findings on CTA and gastric blanching observed during the EGD, she was assumed to have vascular insufficiency likely secondary to vasculitis in light of positive ANCA and lupus anticoagulant. After appropriate treatment the patient was discharged with rheumatologic follow up.
Discussion: This case is presented to educate physicians on a possible manifestation of vascular insufficiency on endoscopy and to always keep it in mind when evaluating a patient presenting with severe abdominal pain. Vascular insufficiency can manifest itself in many ways, but in our case, different clues led us to the diagnosis from her physical exam, to the findings seen on CTA and to the results appreciated on EGD.

Disclosures:
Erika Vigandt, MD1, Denzil Etienne, MD1, Eric Landa, MD2. C0306 - Blanching Gastric Mucosa: An Endoscopic Finding in a Patient With Celiac Artery Occlusion Leading to Vascular Insufficiency, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The Brooklyn Hospital Center, Brooklyn, NY; 2Wyckoff Heights Medical Center, Brooklyn, NY
Introduction: Celiac artery occlusion is a significant and debilitating disorder usually characterized by abdominal pain and diagnosed via radiological imaging modalities. Endoscopic findings in this disease have not been clearly depicted. We present a case with significant endoscopic findings of patchy blanching gastric mucosa induced by insufflation during esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 40 year old woman with past medical history significant for hypertension, intracranial aneurysm with open clipping, coronary artery disease, polyarteritis nodosa presented to the emergency department (ED) complaining of intractable epigastric abdominal pain which had become progressively worse over the past month. Initially, the pain was described as intermittent and crampy which then became constant, 10/10 in intensity, associated with poor oral tolerance, nausea and non-bloody, non-bilious vomiting. Upon presentation vital signs were T 97.9 F, HR 96 bpm, BP 162/117 mmHg, SpO2 99% on room air. On physical exam, patient was ill appearing with diffuse abdominal tenderness with guarding and rebound tenderness, soft, non-distended, with bowel sounds appreciated. Computed tomography angiography (CTA) of the abdomen/pelvis revealed complete occlusion of the celiac artery at the origin and stenosis at the SMA origin with retrograde filling of the celiac territory via an enlarged IPDA collateral. The Gastroenterology service was consulted and an EGD was performed. Upon insufflation of air into the stomach, patchy blanching of the gastric mucosa was noted which continued to worsen, this immediately improved upon deflation. Superficial erosions were also seen in the entire stomach, otherwise the remainder of the exam was normal. Based on the patient’s recent findings on CTA and gastric blanching observed during the EGD, she was assumed to have vascular insufficiency likely secondary to vasculitis in light of positive ANCA and lupus anticoagulant. After appropriate treatment the patient was discharged with rheumatologic follow up.
Discussion: This case is presented to educate physicians on a possible manifestation of vascular insufficiency on endoscopy and to always keep it in mind when evaluating a patient presenting with severe abdominal pain. Vascular insufficiency can manifest itself in many ways, but in our case, different clues led us to the diagnosis from her physical exam, to the findings seen on CTA and to the results appreciated on EGD.

Figure: Patchy blanching of the gastric mucosa with superficial erosions as demonstrated on EGD.
Disclosures:
Erika Vigandt indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Eric Landa indicated no relevant financial relationships.
Erika Vigandt, MD1, Denzil Etienne, MD1, Eric Landa, MD2. C0306 - Blanching Gastric Mucosa: An Endoscopic Finding in a Patient With Celiac Artery Occlusion Leading to Vascular Insufficiency, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
