Back

Poster Session B - Monday Morning
Category: Small Intestine
B0651 - Implicit Bias Contributing to Delayed Diagnosis in a Rare Case of Endoscopic Biopsy Proven Gastrointestinal Amyloidosis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Meghana Ghattu, MD
Abbott Northwestern
Minneapolis, MN
Presenting Author(s)
Meghana Ghattu, MD, Jared Buschette, MD, Breanna Zarmbinski, MD
Abbott Northwestern, Minneapolis, MN
Introduction: Gastrointestinal amyloidosis often requires extensive workup to diagnose, but early diagnosis and initiation of treatment improves mortality1. Implicit bias leads to narrow workups which can misdiagnose rare diseases. We present a case of gastrointestinal amyloidosis ultimately diagnosed by endoscopic biopsy. The rarity of this disease as well as bias that led to anchoring on more common diagnoses resulted in months of misdiagnosis.
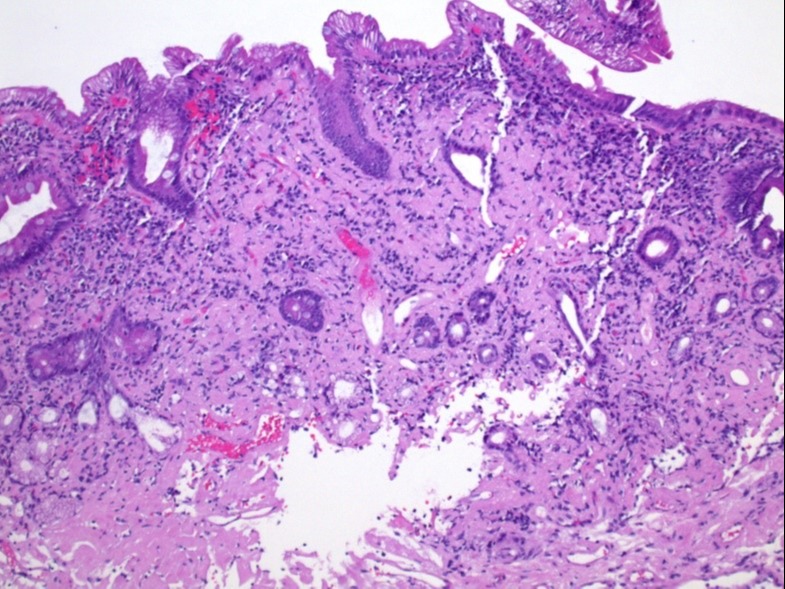
Case Description/Methods: A 67 year old woman with a history of abdominal aortic aneurysm (AAA), substance use disorder in remission, and chronic malnutrition presented with worsening of chronic abdominal pain. Workup over the course of eight prior ED visits for abdominal pain was unremarkable. Her pain was attributed to functional pain or opioid use and withdrawal despite a lack of documented opioid relapse. On this presentation, expanding AAA size prompted surgical consult. The surgical team expressed concern that she would not tolerate an open repair with a BMI of 13.9; TPN was started. GI recommended endoscopy to assess for a malabsorptive process. Unfortunately the procedure was delayed 22 days as the patient felt her uncontrolled pain was not validated by the care team. After many care conferences, she agreed to upper endoscopy which showed flattening of the villi of the duodenum. Microscopic testing from biopsies showed extensive amyloidosis (Fig. 1). Amyloidosis resulting in intestinal ischemia was thought to be the cause of her pain and malnutrition.
Discussion: Implicit bias associated with the patient’s history of addiction led to anchoring bias and initial narrow workup and misdiagnosis. Implicit bias amongst physicians regarding substance use disorders has been associated with suboptimal care2. The severity of the patient’s abdominal pain and malnutrition should have prompted earlier referral to GI and may have led to expedited diagnosis of intestinal amyloidosis. Additionally, the frequent misdiagnosis and dismissal of symptoms resulted in mistrust leading the patient to decline further workup. Recognizing implicit bias can allow clinicians to provide more equitable workup and care.
1. Hasib Sidiqi, M., et al. Immunoglobulin light chain amyloidosis diagnosis and treatment algorithm 2021. 05/21/2021. pp 1-9.
2. Van Boekel, L. C., et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. 07/01/2013. pp 23-35.
Disclosures:
Meghana Ghattu, MD, Jared Buschette, MD, Breanna Zarmbinski, MD. B0651 - Implicit Bias Contributing to Delayed Diagnosis in a Rare Case of Endoscopic Biopsy Proven Gastrointestinal Amyloidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Abbott Northwestern, Minneapolis, MN
Introduction: Gastrointestinal amyloidosis often requires extensive workup to diagnose, but early diagnosis and initiation of treatment improves mortality1. Implicit bias leads to narrow workups which can misdiagnose rare diseases. We present a case of gastrointestinal amyloidosis ultimately diagnosed by endoscopic biopsy. The rarity of this disease as well as bias that led to anchoring on more common diagnoses resulted in months of misdiagnosis.
Case Description/Methods: A 67 year old woman with a history of abdominal aortic aneurysm (AAA), substance use disorder in remission, and chronic malnutrition presented with worsening of chronic abdominal pain. Workup over the course of eight prior ED visits for abdominal pain was unremarkable. Her pain was attributed to functional pain or opioid use and withdrawal despite a lack of documented opioid relapse. On this presentation, expanding AAA size prompted surgical consult. The surgical team expressed concern that she would not tolerate an open repair with a BMI of 13.9; TPN was started. GI recommended endoscopy to assess for a malabsorptive process. Unfortunately the procedure was delayed 22 days as the patient felt her uncontrolled pain was not validated by the care team. After many care conferences, she agreed to upper endoscopy which showed flattening of the villi of the duodenum. Microscopic testing from biopsies showed extensive amyloidosis (Fig. 1). Amyloidosis resulting in intestinal ischemia was thought to be the cause of her pain and malnutrition.
Discussion: Implicit bias associated with the patient’s history of addiction led to anchoring bias and initial narrow workup and misdiagnosis. Implicit bias amongst physicians regarding substance use disorders has been associated with suboptimal care2. The severity of the patient’s abdominal pain and malnutrition should have prompted earlier referral to GI and may have led to expedited diagnosis of intestinal amyloidosis. Additionally, the frequent misdiagnosis and dismissal of symptoms resulted in mistrust leading the patient to decline further workup. Recognizing implicit bias can allow clinicians to provide more equitable workup and care.
1. Hasib Sidiqi, M., et al. Immunoglobulin light chain amyloidosis diagnosis and treatment algorithm 2021. 05/21/2021. pp 1-9.
2. Van Boekel, L. C., et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. 07/01/2013. pp 23-35.
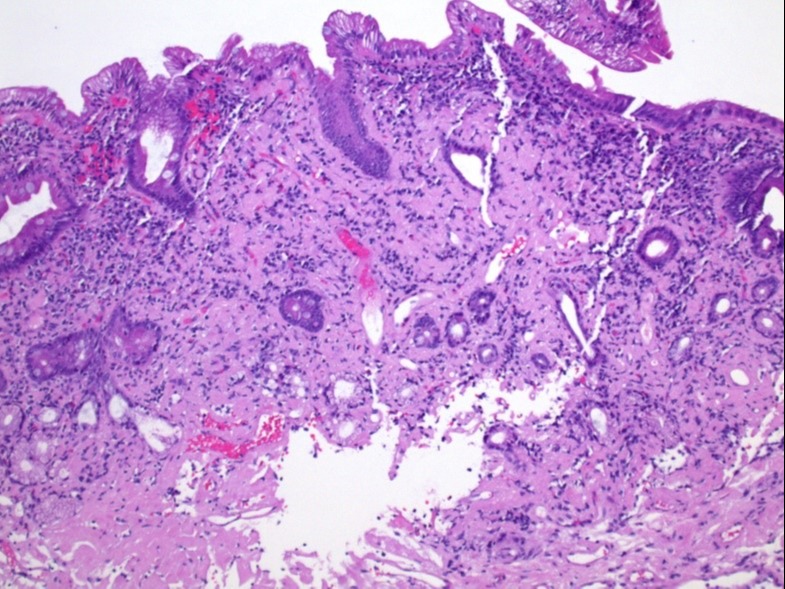
Figure: Figure 1: DUODENUM, BIOPSY
Amyloidosis, extensive, involving mucosa and submucosa, perivascular and diffuse.
Amyloidosis, extensive, involving mucosa and submucosa, perivascular and diffuse.
Disclosures:
Meghana Ghattu indicated no relevant financial relationships.
Jared Buschette indicated no relevant financial relationships.
Breanna Zarmbinski indicated no relevant financial relationships.
Meghana Ghattu, MD, Jared Buschette, MD, Breanna Zarmbinski, MD. B0651 - Implicit Bias Contributing to Delayed Diagnosis in a Rare Case of Endoscopic Biopsy Proven Gastrointestinal Amyloidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
