Back

Poster Session B - Monday Morning
Category: Small Intestine
B0653 - Recurrent Small Bowel Perforation due to IgG4 Mediated Enteropathy
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Seth Haydel, MD
Leonard J. Chabert Medical Center
Houma, Louisiana
Presenting Author(s)
Seth Haydel, MD1, Babiswarup Chandamuri, MD2, Catherine Hudson, MD, MPH3
1Leonard J. Chabert Medical Center, Houma, LA; 2South Louisiana Medical Associates, Houma, LA; 3Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Small bowel perforation is a rare but serious complication from causes such as trauma, neoplasm, obstruction, or complications from IBD. We present a case of recurrent small bowel perforation due to IgG4 mediated enteropathy (IME).
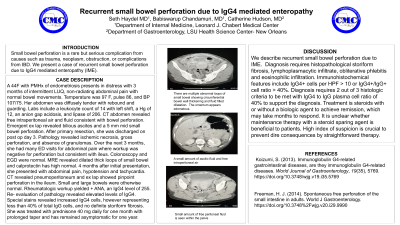
Case Description/Methods: A 44F with PMHx of endometriosis presents in distress with 3 months of intermittent LUQ, non-radiating abdominal pain with normal bowel movements. Temperature was 97 F, pulse 86, and BP 107/75. Her abdomen was diffusely tender with rebound and guarding. Labs include a leukocyte count of 14 with left shift, a Hg of 12, an anion gap acidosis, and lipase of 206. CT abdomen revealed free intraperitoneal air and fluid consistent with bowel perforation. Emergent ex lap revealed bilious ascites and a 5 mm mid small bowel perforation. After primary resection, she was discharged on post op day 3. Pathology revealed ischemic necrosis, gross perforation, and absence of granulomas. Over the next 3 months, she had many ED visits for abdominal pain where workup was negative for perforation but consistent with ileus. Colonoscopy and EGD were normal. MRE revealed dilated thick loops of small bowel and calprotectin has high normal. 4 months after initial presentation, she presented with abdominal pain, hypotension and tachycardia. CT revealed pneumoperitoneum and ex lap showed pinpoint perforation in the ileum. Small and large bowels were otherwise normal. Rheumatologic workup yielded + ANA, an IgG4 level of 255. Re- evaluation of pathology revealed elevated levels of IgG4. Special stains revealed increased IgG4 cells, however representing less than 40% of total IgG cells, and no definite storiform fibrosis. She was treated with prednisone 40 mg daily for one month with prolonged taper and has remained asymptomatic for one year.
Discussion: We describe recurrent small bowel perforation due to IME. Diagnosis requires histopathological storiform fibrosis, lymphoplasmacytic infiltrate, obliterative phlebitis and eosinophilic infiltration. Immunohistochemical features include IgG4+ cells per HPF > 10 or IgG4+/IgG+ cell ratio > 40%. Diagnosis requires 2 out of 3 histologic criteria to be met with IgG4 to IgG plasma cell ratio of 40% to support the diagnosis. Treatment is steroids with or without a biologic agent to achieve remission, which may take months to respond. It is unclear whether maintenance therapy with a steroid sparing agent is beneficial to patients. High index of suspicion is crucial to prevent dire consequences by straightforward therapy.
Disclosures:
Seth Haydel, MD1, Babiswarup Chandamuri, MD2, Catherine Hudson, MD, MPH3. B0653 - Recurrent Small Bowel Perforation due to IgG4 Mediated Enteropathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Leonard J. Chabert Medical Center, Houma, LA; 2South Louisiana Medical Associates, Houma, LA; 3Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Small bowel perforation is a rare but serious complication from causes such as trauma, neoplasm, obstruction, or complications from IBD. We present a case of recurrent small bowel perforation due to IgG4 mediated enteropathy (IME).
Case Description/Methods: A 44F with PMHx of endometriosis presents in distress with 3 months of intermittent LUQ, non-radiating abdominal pain with normal bowel movements. Temperature was 97 F, pulse 86, and BP 107/75. Her abdomen was diffusely tender with rebound and guarding. Labs include a leukocyte count of 14 with left shift, a Hg of 12, an anion gap acidosis, and lipase of 206. CT abdomen revealed free intraperitoneal air and fluid consistent with bowel perforation. Emergent ex lap revealed bilious ascites and a 5 mm mid small bowel perforation. After primary resection, she was discharged on post op day 3. Pathology revealed ischemic necrosis, gross perforation, and absence of granulomas. Over the next 3 months, she had many ED visits for abdominal pain where workup was negative for perforation but consistent with ileus. Colonoscopy and EGD were normal. MRE revealed dilated thick loops of small bowel and calprotectin has high normal. 4 months after initial presentation, she presented with abdominal pain, hypotension and tachycardia. CT revealed pneumoperitoneum and ex lap showed pinpoint perforation in the ileum. Small and large bowels were otherwise normal. Rheumatologic workup yielded + ANA, an IgG4 level of 255. Re- evaluation of pathology revealed elevated levels of IgG4. Special stains revealed increased IgG4 cells, however representing less than 40% of total IgG cells, and no definite storiform fibrosis. She was treated with prednisone 40 mg daily for one month with prolonged taper and has remained asymptomatic for one year.
Discussion: We describe recurrent small bowel perforation due to IME. Diagnosis requires histopathological storiform fibrosis, lymphoplasmacytic infiltrate, obliterative phlebitis and eosinophilic infiltration. Immunohistochemical features include IgG4+ cells per HPF > 10 or IgG4+/IgG+ cell ratio > 40%. Diagnosis requires 2 out of 3 histologic criteria to be met with IgG4 to IgG plasma cell ratio of 40% to support the diagnosis. Treatment is steroids with or without a biologic agent to achieve remission, which may take months to respond. It is unclear whether maintenance therapy with a steroid sparing agent is beneficial to patients. High index of suspicion is crucial to prevent dire consequences by straightforward therapy.
Disclosures:
Seth Haydel indicated no relevant financial relationships.
Babiswarup Chandamuri indicated no relevant financial relationships.
Catherine Hudson indicated no relevant financial relationships.
Seth Haydel, MD1, Babiswarup Chandamuri, MD2, Catherine Hudson, MD, MPH3. B0653 - Recurrent Small Bowel Perforation due to IgG4 Mediated Enteropathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
