Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0187 - Underneath the Surface: EUS-Guided Treatment of Varices When Not Endoscopically Visualized
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- AE
Abbinaya Elangovan, MD
University Hospitals Cleveland Medical Center/ Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abbinaya Elangovan, MD1, Vibhu Chittajallu, MD2, Adam Loutfy, DO3, Sagarika Satyavada, MD2, Amitabh Chak, MD4, Ashley L. Faulx, MD5, Brooke Glessing, MD1, Gerard Isenberg, MD2
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2University Hospitals Case Medical Center/ Case Western Reserve University, Cleveland, OH; 3University Hospitals, Cleveland, OH; 4University Hospitals, Digestive Health Institute, Cleveland, OH; 5Louis Stokes Cleveland VA Medical Center, University Hospitals, Case Western Reserve University, Cleveland, OH
Introduction: Endoscopic visualization of varices can be challenging in some clinical scenarios. Here we describe three cases in which endoscopic ultrasound (EUS) was used to identify and treat varices.
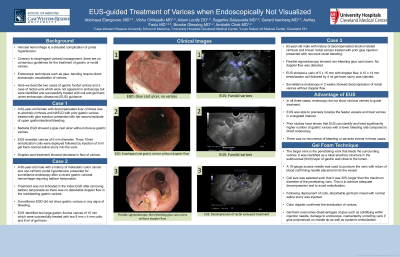
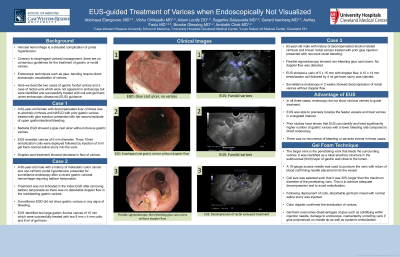
Case Description/Methods: Case 1
A 62-year-old female with decompensated cirrhosis and isolated gastric fundal varices treated with prior glue injection presented with her second episode of upper gastrointestinal (GI) bleeding. Urgent esophagogastroduodenoscopy (EGD) showed a glue cast ulcer without obvious gastric varices. EUS revealed tubal, anechoic structures in the fundus of the stomach consistent with varices. A 19-gauge access needle was used to puncture the varices with return of blood flow. Three 10mm embolization coils followed by 8 ml of gel foam-normal saline slurry were injected into the varix. Doppler post-treatment showed a decrease in the flow of the treated varix and of the deeper varices.
Case 2:
A 60-year-old male with non-cirrhotic portal hypertension from portal vein thrombosis was admitted for hemorrhagic shock from gastric variceal hemorrhage. Endoscopic evaluation showed non-bleeding gastroesophageal varices. Surveillance endoscopy one week later showed no obvious gastric varices, but EUS identified two large gastric fundus varices which were treated with two 8 mm coil and 8 ml gel foam. Complete thrombosis of both varices was noted. Surveillance EUS-guided treatment was performed until eradication without recurrence.
Case 3:
A 63-year-old male with decompensated cirrhosis presented with recurrent rectal variceal bleeding after previous treatment with glue injection. Flexible sigmoidoscopy showed few glue cast rectal ulcers with no obvious bleeding. EUS showed a varix of 5 x 15 mm which was treated with a 10 x 14 mm embolization coil and 4 ml of gel-foam normal saline slurry leading to eradication. Surveillance endoscopy in two weeks showed decompression of rectal varices.
Discussion: In all three cases, EGD performed for recent gastrointestinal bleeding did not show any evidence of varices. However, EUS could precisely localize the feeder vessels, verify the needle placement into the vessel by aspirating blood and inject coils followed by gel foam into varices in a targeted manner. Successful treatment of varices was confirmed by the decrease in Doppler flow of the treated varices. No post-procedure adverse events such as pain, bleeding or embolization were noted. This illustrates the utility of EUS in the treatment of varices when they are not detected endoscopically.
Disclosures:
Abbinaya Elangovan, MD1, Vibhu Chittajallu, MD2, Adam Loutfy, DO3, Sagarika Satyavada, MD2, Amitabh Chak, MD4, Ashley L. Faulx, MD5, Brooke Glessing, MD1, Gerard Isenberg, MD2. B0187 - Underneath the Surface: EUS-Guided Treatment of Varices When Not Endoscopically Visualized, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2University Hospitals Case Medical Center/ Case Western Reserve University, Cleveland, OH; 3University Hospitals, Cleveland, OH; 4University Hospitals, Digestive Health Institute, Cleveland, OH; 5Louis Stokes Cleveland VA Medical Center, University Hospitals, Case Western Reserve University, Cleveland, OH
Introduction: Endoscopic visualization of varices can be challenging in some clinical scenarios. Here we describe three cases in which endoscopic ultrasound (EUS) was used to identify and treat varices.
Case Description/Methods: Case 1
A 62-year-old female with decompensated cirrhosis and isolated gastric fundal varices treated with prior glue injection presented with her second episode of upper gastrointestinal (GI) bleeding. Urgent esophagogastroduodenoscopy (EGD) showed a glue cast ulcer without obvious gastric varices. EUS revealed tubal, anechoic structures in the fundus of the stomach consistent with varices. A 19-gauge access needle was used to puncture the varices with return of blood flow. Three 10mm embolization coils followed by 8 ml of gel foam-normal saline slurry were injected into the varix. Doppler post-treatment showed a decrease in the flow of the treated varix and of the deeper varices.
Case 2:
A 60-year-old male with non-cirrhotic portal hypertension from portal vein thrombosis was admitted for hemorrhagic shock from gastric variceal hemorrhage. Endoscopic evaluation showed non-bleeding gastroesophageal varices. Surveillance endoscopy one week later showed no obvious gastric varices, but EUS identified two large gastric fundus varices which were treated with two 8 mm coil and 8 ml gel foam. Complete thrombosis of both varices was noted. Surveillance EUS-guided treatment was performed until eradication without recurrence.
Case 3:
A 63-year-old male with decompensated cirrhosis presented with recurrent rectal variceal bleeding after previous treatment with glue injection. Flexible sigmoidoscopy showed few glue cast rectal ulcers with no obvious bleeding. EUS showed a varix of 5 x 15 mm which was treated with a 10 x 14 mm embolization coil and 4 ml of gel-foam normal saline slurry leading to eradication. Surveillance endoscopy in two weeks showed decompression of rectal varices.
Discussion: In all three cases, EGD performed for recent gastrointestinal bleeding did not show any evidence of varices. However, EUS could precisely localize the feeder vessels, verify the needle placement into the vessel by aspirating blood and inject coils followed by gel foam into varices in a targeted manner. Successful treatment of varices was confirmed by the decrease in Doppler flow of the treated varices. No post-procedure adverse events such as pain, bleeding or embolization were noted. This illustrates the utility of EUS in the treatment of varices when they are not detected endoscopically.
Disclosures:
Abbinaya Elangovan indicated no relevant financial relationships.
Vibhu Chittajallu indicated no relevant financial relationships.
Adam Loutfy indicated no relevant financial relationships.
Sagarika Satyavada indicated no relevant financial relationships.
Amitabh Chak indicated no relevant financial relationships.
Ashley Faulx indicated no relevant financial relationships.
Brooke Glessing indicated no relevant financial relationships.
Gerard Isenberg indicated no relevant financial relationships.
Abbinaya Elangovan, MD1, Vibhu Chittajallu, MD2, Adam Loutfy, DO3, Sagarika Satyavada, MD2, Amitabh Chak, MD4, Ashley L. Faulx, MD5, Brooke Glessing, MD1, Gerard Isenberg, MD2. B0187 - Underneath the Surface: EUS-Guided Treatment of Varices When Not Endoscopically Visualized, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
