Back

Poster Session B - Monday Morning
Category: Endoscopy Video Forum
B0191 - Accessing the Bile Duct: Not the Usual Way
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Zunirah Ahmed, MD
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Zunirah Ahmed, MD1, Abdullah Cheema, 2, Sammak Cheema, 2, Ali Raza, MD1
1Houston Methodist Hospital, Houston, TX; 2Texas A&M, College Station, TX
Introduction: Percutaneous transhepatic cholangioscopy (PTCS) provides direct visualization of the biliary system. Direct visualization of the biliary system has advantages for the identification and treatment of intraductal lesions compared to indirect imaging of endoscopic retrograde cholangiopancreatography (ERCP). This case highlights the role of PTSC in diagnosis of cholangiocarcinoma.
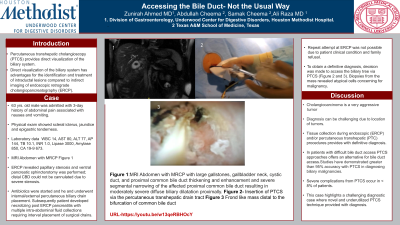
Case Description/Methods: 63 yrs old male was admitted with 3 day history of abdominal pain associated with nausea and vomiting. Physical exam was remarkable for scleral icterus, jaundice and epigastric tenderness. Laboratory data showed WBC 14, AST 80, ALT 77, AP 144, TB 10.1, INR 1.0, Lipase 3000, Amylase 850, CA 19-9 673.MRI Abdomen with MRCP revealed large gallstones in the gallbladder neck, and proximal CBD obstruction with severe diffuse biliary dilatation proximally(Figure 1); no definite stricture was noted. ERCP revealed papillary stenosis and ventral pancreatic sphincterotomy was performed; distal CBD could not be cannulated due to severe stenosis. He was started on antibiotics and underwent internal/external percutaneous biliary drain placement. He subsequently developed necrotizing post ERCP pancreatitis with multiple intra-abdominal fluid collections requiring interval placement of surgical drains. He had a complicated hospital course requiring mechanical ventilation and dialysis.Repeat attempt at ERCP was not possible due to patient clinical condition and family refusal. To obtain a definitive diagnosis, decision was made to access the biliary tree via PTSC. Biopsies from the mass revealed atypical cells concerning for malignancy.Patient and family decided to opt for hospice.
Discussion: Cholangiocarcinoma is a very aggressive tumor which can be classified as intrahepatic, peri-hilar and distal based on location. Diagnosis can be challenging due to location of tumors. Tissue collection during endoscopic (ERCP) and/or percutaneous transhepatic (PTC) procedures provides with definitive diagnosis. In patients with difficult bile duct access PTSC approaches offers an alternative for bile duct access. Studies have demonstrated greater than 95% accuracy with PTCS in diagnosing biliary malignancies. Overall, PTCS is a safe and effective procedure, with severe complications occurring in less than 8% of patients. This case highlights a challenging diagnostic case where novel and underutilized PTSC technique provided with diagnosis.

Disclosures:
Zunirah Ahmed, MD1, Abdullah Cheema, 2, Sammak Cheema, 2, Ali Raza, MD1. B0191 - Accessing the Bile Duct: Not the Usual Way, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Texas A&M, College Station, TX
Introduction: Percutaneous transhepatic cholangioscopy (PTCS) provides direct visualization of the biliary system. Direct visualization of the biliary system has advantages for the identification and treatment of intraductal lesions compared to indirect imaging of endoscopic retrograde cholangiopancreatography (ERCP). This case highlights the role of PTSC in diagnosis of cholangiocarcinoma.
Case Description/Methods: 63 yrs old male was admitted with 3 day history of abdominal pain associated with nausea and vomiting. Physical exam was remarkable for scleral icterus, jaundice and epigastric tenderness. Laboratory data showed WBC 14, AST 80, ALT 77, AP 144, TB 10.1, INR 1.0, Lipase 3000, Amylase 850, CA 19-9 673.MRI Abdomen with MRCP revealed large gallstones in the gallbladder neck, and proximal CBD obstruction with severe diffuse biliary dilatation proximally(Figure 1); no definite stricture was noted. ERCP revealed papillary stenosis and ventral pancreatic sphincterotomy was performed; distal CBD could not be cannulated due to severe stenosis. He was started on antibiotics and underwent internal/external percutaneous biliary drain placement. He subsequently developed necrotizing post ERCP pancreatitis with multiple intra-abdominal fluid collections requiring interval placement of surgical drains. He had a complicated hospital course requiring mechanical ventilation and dialysis.Repeat attempt at ERCP was not possible due to patient clinical condition and family refusal. To obtain a definitive diagnosis, decision was made to access the biliary tree via PTSC. Biopsies from the mass revealed atypical cells concerning for malignancy.Patient and family decided to opt for hospice.
Discussion: Cholangiocarcinoma is a very aggressive tumor which can be classified as intrahepatic, peri-hilar and distal based on location. Diagnosis can be challenging due to location of tumors. Tissue collection during endoscopic (ERCP) and/or percutaneous transhepatic (PTC) procedures provides with definitive diagnosis. In patients with difficult bile duct access PTSC approaches offers an alternative for bile duct access. Studies have demonstrated greater than 95% accuracy with PTCS in diagnosing biliary malignancies. Overall, PTCS is a safe and effective procedure, with severe complications occurring in less than 8% of patients. This case highlights a challenging diagnostic case where novel and underutilized PTSC technique provided with diagnosis.

Figure: MRI Abdomen with MRCP with large gallstones, Gallbladder neck, cystic duct, and proximal common bile duct thickening and enhancement and severe segmental narrowing of the affected proximal common bile duct resulting in moderately severe diffuse biliary dilatation proximally.
Disclosures:
Zunirah Ahmed indicated no relevant financial relationships.
Abdullah Cheema indicated no relevant financial relationships.
Sammak Cheema indicated no relevant financial relationships.
Ali Raza indicated no relevant financial relationships.
Zunirah Ahmed, MD1, Abdullah Cheema, 2, Sammak Cheema, 2, Ali Raza, MD1. B0191 - Accessing the Bile Duct: Not the Usual Way, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
